Did you know that nearly 28 million cataract procedures take place annually worldwide? That’s about 75,000 procedures every day. The tiny artificial lenses used in these surgeries, called intraocular lenses (IOLs), replace the eye’s natural lens during cataract surgery to restore clear vision.
Surgeons craft these cataract replacement lenses from biocompatible materials that safely integrate with the human eye. Silicone and acrylic compositions make up the most common types of cataract lenses. Silicone-based IOLs provide excellent flexibility and durability, while acrylic intraocular lenses deliver superior optical clarity and resist deposits better over time. Most cataract lenses also feature special protective coatings that shield the eyes from harmful ultraviolet rays.
The science behind cataract lens materials shows remarkable progress in implant technology. Modern flexible IOLs slide through tiny incisions without requiring stitches. This advancement makes the procedure quick – typically under 30 minutes – yet delivers life-changing results for patients.
The Evolution of Intraocular Lens Materials
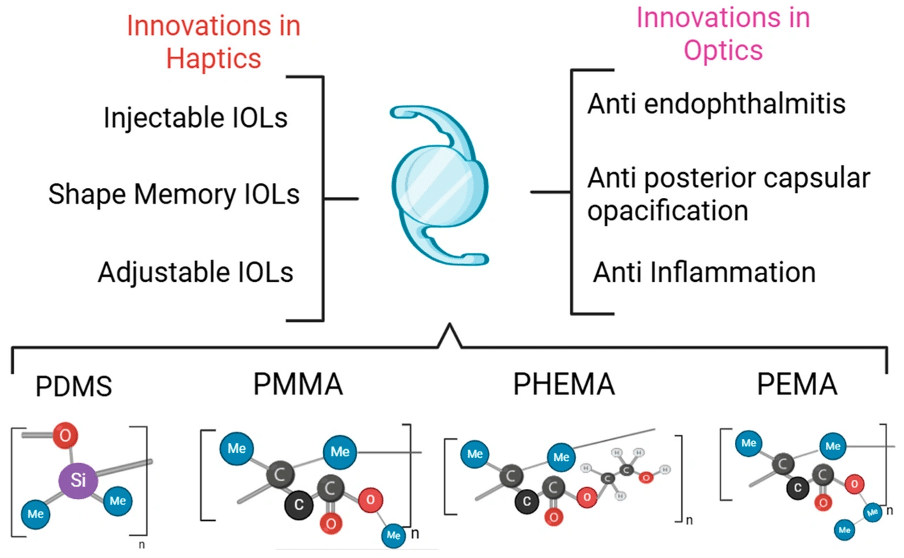
Image Source: MDPI
Sir Harold Ridley started the development of cataract lens materials in 1949 by implanting the first intraocular lens (IOL) made from polymethyl methacrylate (PMMA). His revolutionary material choice stemmed from wartime observations that Plexiglas fragments from aircraft windshields stayed inert in pilots’ eyes.
From PMMA to Modern Biomaterials
PMMA ruled the IOL world for over 30 years and provided excellent biocompatibility, outstanding optical properties, and high light transmissibility. Its rigidity required large incisions (5-7mm) that needed stitching, which led to longer recovery times and potential astigmatism.
Charles Kelman’s introduction of phacoemulsification in the 1970s marked a turning point that reduced incision sizes and drove material diversification. The 1980s saw the emergence of foldable silicone IOLs, and later came hydrophobic and hydrophilic acrylic materials. These new materials allowed smaller incisions (as small as 1.8mm for some hydrophilic lenses) and improved surgical outcomes dramatically.
Key Properties of Effective IOL Materials
Cataract replacement lenses need several significant characteristics to work well. Biocompatibility will give a minimal inflammatory response within the eye. Optical clarity determines visual quality, and PMMA has shown the highest transparency across visible light ranges.
The refractive index should ideally approach 1.4 (the natural lens value). Modern hydrophobic acrylics reach indices of 1.44-1.55, which allows for thinner lens designs. Glass transition temperature (Tg) plays a vital role as the point where materials change from rigid to flexible states. IOLs must maintain a Tg below body temperature (37°C) to unfold properly after implantation.
UV-Filtering Components in Modern Lenses
The natural crystalline lens philtres harmful ultraviolet radiation, particularly in the 300-400nm range. Modern intra ocular lenses include UV-blocking components to restore this protection after cataract surgery removes the natural lens. This protection helps prevent potential retinal photochemical damage.
Advanced cataract lenses now include blue-light filtering technology. Hoya in Japan developed these yellow-pigmented IOLs to reduce short-wavelength light exposure that might contribute to age-related macular degeneration. Patients initially see blue-tinted vision (cyanopsia) with these lenses before adapting.
Primary Materials Used in Cataract Lenses Today

Image Source: ScienceDirect.com
Today’s intraocular lens (IOL) market features four main materials. Each has unique properties that make them perfect for different patient needs. These materials have come a long way from the old rigid PMMA lenses.
Hydrophobic Acrylic: Properties and Benefits
Hydrophobic acrylic IOLs lead the global market share. Made from esters of poly(meth)acrylic acid, these lenses take in less than 1% water but stay flexible even when dry. Their high refractive index (1.47-1.55) helps create thinner lens designs. The sticky surface of hydrophobic materials sticks well to the capsular bag through fibronectin bindings and gives better rotational stability. So, these lenses show lower rates of posterior capsule opacification (PCO) than hydrophilic options. New versions like the Vivinex iSert XY1 and Clareon SY60WF have smoother surfaces that might reduce cell adhesion even more. But despite these benefits, some hydrophobic materials can develop glistenings—tiny fluid-filled spaces that scatter light and might affect vision.
Hydrophilic Acrylic: Applications and Advantages
About 29% of IOLs implanted worldwide are hydrophilic acrylic lenses. We made these from poly(2-hydroxyethyl methacrylate) hydrogels with 18-38% water content. Their high water content makes them extremely biocompatible and great for patients with uveitis or diabetes. These IOLs unfold smoothly in the eye, which gives surgeons better control during placement. You can insert them through tiny 1.8mm incisions because they’re more flexible and compressible—perfect for microincision cataract surgery. These lenses resist surface damage better and show fewer glistenings than hydrophobic ones. The biggest problem is their lower refractive index (around 1.41-1.44), which means they need to be thicker.
Silicone-Based IOLs: When They’re Recommended
Silicone IOLs, made mostly from polydimethylsiloxane (PDMS), were the first foldable lenses doctors used clinically. These super-hydrophobic materials (contact angle 99°) are clear, flexible, and heat-resistant. Research shows that sharp-edged silicone IOLs work great at stopping PCO formation over long periods. But they do have some unique challenges. Silicone materials stick strongly to silicone oil used in vitreoretinal surgery, which can make it hard to see. They also unfold faster in the eye, which might make placement trickier. Silicone remains a good choice for patients who probably won’t need posterior segment procedures later.
Collamer: The Biocompatible Hybrid Material
STAAR Surgical’s EVO ICL products exclusively use Collamer, an innovative hybrid material. This special copolymer blends hydroxyethyl methacrylate (60%), water (36%), benzophenone (3.8%), and porcine collagen (0.2%). Adding collagen—that’s where the name “Collamer” comes from—makes the lens more biocompatible and lighter. The material’s structure helps exchange gases and nutrients while protecting against UV light. Though mainly used in phakic IOLs instead of cataract replacement, Collamer works exceptionally well with eye tissues. Its soft, flexible nature makes it easier to implant and reduces iris irritation and endothelial damage.
Also Read: How to Prevent Cataracts: A London Eye Surgeon’s Natural Solutions
How IOL Materials Affect Patient Outcomes
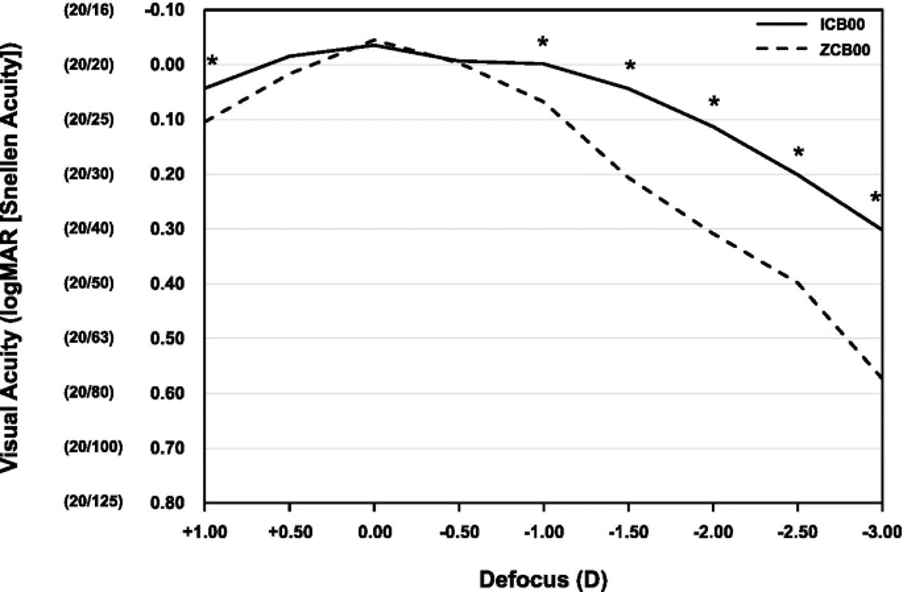
Image Source: BMC Ophthalmology – BioMed Central
The way cataract lenses are made has a direct effect on how well patients do after surgery. Good vision after surgery depends on several factors beyond just the lens material.
Biocompatibility and Tissue Response
The eye’s tolerance of an intraocular lens (IOL) shows its biocompatibility. This covers uveal biocompatibility (inflammatory response) and capsular biocompatibility (interaction with lens epithelial cells). Research shows that hydrophilic acrylic IOLs work better with uveal tissue because they have more water content. All the same, hydrophobic materials tend to work better with the capsular tissue. The sticky surface of hydrophobic IOLs bonds strongly with fibronectin in the capsular bag and leaves less room for cells to move around.
Clarity and Light Transmission Properties
The quality of vision after surgery depends on optical clarity. PMMA has been the leader in letting visible light through. Hydrophilic acrylic IOLs face a big challenge – they can calcify. Calcium phosphate deposits can cut light transmission by more than 40% in affected lenses. Hydrophobic acrylics sometimes develop glistenings (tiny pockets filled with fluid), especially when they have less water content. These scatter light and might reduce contrast sensitivity, but rarely affect how well people see in normal light.
Flexibility and Surgical Insertion Techniques
Modern IOLs are flexible enough to fit through tiny 1.8mm incisions. Surgeons use both hands to insert the lens while keeping the eye centred. The lens position matters for good vision—recent studies show modern lenses typically shift just 0.11mm side-to-side and 0.03mm up-and-down. Heavier lenses tend to move more in very nearsighted eyes.
Long-Term Stability and Posterior Capsule Opacification Rates
Different materials lead to different long-term results. PCO happens in 18% of cases after three years and 31% after five years. Foldable IOLs need fewer Nd:YAG capsulotomies (14.1%) than rigid ones (31.1%). Among foldable materials, hydrophobic acrylic IOLs have the lowest PCO rates—Alcon Acrysof sees just 0.9% compared to 17.1% with other designs. These better results come from the square-edged design and sticky properties that create a barrier.
Manufacturing Processes for Cataract Replacement Lenses
Raw biomaterials must go through specialised manufacturing processes to become precision optical implants. These processes must deliver optical perfection and biocompatibility. The evolution of intraocular lenses (IOLs) manufacturing techniques has grown with material science.
Precision Moulding Techniques
We used two methods to make cataract replacement lenses: injection moulding and diamond cutting/turning. Cast moulding, a type of injection moulding, is accessible to more people because it reduces production time by approximately 70% and allows different lens shapes. Polypropylene moulding bodies (male and female components) create the basic lens geometry.
The success of injection moulding depends on several factors. These include melt temperature (210-250°C), mould temperature (60-90°C), injection pressure (50-70 MPa), and cooling time (15-45 seconds). These factors directly affect the volumetric shrinkage of the lens, which averages 4.29% under ideal conditions.
Manufacturers face unique challenges with hydrophobic acrylic IOLs. The soft biomaterial can deform during cutting and create surface form errors. Electrorheological polishing offers a solution. This non-contact method employs electrorheological fluid under electric field conditions to improve surface quality to nanometre roughness levels.
Surface Treatments and Coatings
IOLs need various surface modifications after moulding to work better. Hydrophilic coatings create a slippery layer that makes insertion easier through tiny incisions. These coatings protect the lens’s delicate structure during implantation.
New approaches show promise. Photodynamic coatings with chlorin e6 photosensitizers can eliminate remaining lens epithelial cells when light activates them. This reduces posterior capsule opacification. Mussel-inspired coatings that have photothermal properties can also stop lens epithelial cells. They do this by raising temperature (50-60°C) when exposed to near-infrared laser irradiation.
Quality Control in IOL Production
ISO class 7 or 8 cleanrooms are where cataract replacement lenses are made. Each lens undergoes strict testing to meet optical and dimensional specifications. Quality control checks include:
- Optical testing for clarity and light transmission
- Validation of refractive power and focal properties
- Dimensional inspection for precise measurements
- Surface examination for defects or irregularities
Traditional polishing methods result in qualification rates of only 30% or lower. Advanced manufacturing processes have improved quality consistency by a lot. Every IOL goes through sterilisation, usually with ethylene oxide gas or gamma radiation, before being sealed in sterile containers.
Also Read: Single vs Double Cataract Surgery: What London Specialists Recommend
Conclusion
Understanding the Impact of IOL Materials on Vision Restoration
Sir Harold Ridley’s pioneering PMMA implants marked the beginning of a remarkable journey that led to today’s sophisticated biomaterials. Without doubt, this progress stands as one of ophthalmology’s greatest achievements. Cataract surgery has grown from just preserving vision to giving patients a chance to see better than before.
Modern IOL materials do much more than just provide transparency. Each material offers unique benefits based on what individual patients need. Hydrophobic acrylics stand out with their stability and PCO resistance. Hydrophilic materials work better for patients with inflammatory conditions. Silicone lenses still have their place in specific cases, while the innovative Collamer shows how hybrid materials could reshape future developments.
The science behind these lens materials affects patient outcomes in many ways. Physical properties guide surgeons’ techniques and determine incision sizes. The body’s response depends on how compatible these materials are with human tissue. Visual quality and issues like glistenings or calcification link directly to the optical characteristics of these materials.
Precision in manufacturing is vital to how well IOLs perform. These tiny implants must meet exact standards since they’ll stay in the eye for life. This requires advanced moulding techniques, special surface treatments, and strict quality checks.
Cataract surgery keeps getting better, and new materials lead the way. Scientists are working on surfaces enhanced with nanotechnology, lenses that can release drugs, and materials that might move like natural lenses. These aren’t just clear discs – they’re complex devices that bring together material science, precise engineering, and medical breakthroughs to restore our most precious sense.
FAQs
Q1. How long do intraocular lenses (IOLs) typically last after cataract surgery? Intraocular lenses are designed to be permanent implants. Unlike natural lenses, IOLs do not degrade over time and are expected to last for the remainder of a patient’s life once implanted.
Q2. What are the primary materials used in modern cataract lenses? Modern cataract lenses are primarily made from four materials: hydrophobic acrylic, hydrophilic acrylic, silicone, and Collamer. Each material has unique properties that make it suitable for different patient needs and surgical scenarios.
Q3. How do different IOL materials affect patient outcomes? The choice of IOL material can impact various aspects of patient outcomes, including biocompatibility, optical clarity, flexibility for surgical insertion, and long-term stability. For instance, hydrophobic acrylic lenses often show lower rates of posterior capsule opacification compared to other materials.
Q4. Are there any special coatings or treatments applied to cataract lenses? Yes, many cataract lenses receive special surface treatments or coatings. These can include UV-blocking components to protect the retina, hydrophilic coatings to ease insertion, and in some cases, blue-light filtering technology to reduce short-wavelength light exposure.
Q5. How are intraocular lenses manufactured to ensure quality and precision? Cataract lenses are manufactured using precision moulding techniques in controlled cleanroom environments. The process involves strict quality control measures, including optical testing, dimensional inspection, and surface examination. Advanced manufacturing processes have significantly improved consistency and quality in IOL production.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

