Nearly 30.3 million people in the United Kingdom have diabetes, and diabetic patients make up 20% of all cataract surgeries. These patients need substantially more attention and specialised care than standard procedures. High blood sugar levels change lens proteins, which speeds up cataract formation and makes symptoms worse faster.
Diabetes and cataracts create unique challenges during surgery and recovery. Your risk of complications like retinal detachment, vitreous haemorrhage, and infections increases substantially. Blood sugar control plays a vital role before surgery. Medical experts recommend keeping fasting levels below 140 mg/dL to reduce risks. Diabetes and cataracts share a complex connection. Your success depends on detailed preoperative evaluation, careful surgical planning, and close monitoring after the procedure. This piece shows you everything you need to know about safe and effective cataract surgery, especially when you have diabetes. Expert care makes a real difference in your outcome.

Preoperative Evaluation for Diabetic Cataract Patients
Doctors must fully review diabetic patients before cataract surgery to achieve the best possible vision outcomes. Diabetes makes cataracts develop faster, with rates five times higher than in non-diabetic patients. These patients develop cataracts earlier, usually showing posterior subcapsular opacities.
Assessing diabetic retinopathy and macular oedema
Eye doctors need these detailed tests for diabetic cataract patients:
- Visual acuity and best-corrected visual acuity assessment
- Dilated fundus examination to look for retinopathy signs
- Slit-lamp biomicroscopy to check anterior segment health
- Gonioscopy to check for neovascularization
- Tonometry to measure intraocular pressure
Doctors use advanced tests like optical coherence tomography (OCT) and fluorescein angiography in complex cases to spot subtle macular changes. Research shows patients who already have diabetic macular oedema (DME) face higher risks of post-operative macular oedema, with progression rates between 20% to 50%. Poor vision outcomes strongly associate with clinically significant macular oedema (CSME) during surgery.
Pre-existing proliferative diabetic retinopathy (PDR) gets worse faster after cataract surgery. Doctors should perform panretinal photocoagulation (PRP) before surgery. Dense cataracts might block proper retinal treatment, so PRP can happen right after surgery.

HbA1c and blood glucose targets before surgery
The need for strict blood sugar control before cataract surgery lacks clear evidence about specific HbA1c limits. The Royal College of Ophthalmologists hasn’t found enough proof to cancel surgery above any particular blood sugar or HbA1c level. UK guidelines accept a preoperative HbA1c <8.5% (69 mmol/mol) for surgery. Better long-term blood sugar control definitely reduces diabetic problems including retinopathy and cataracts. The decision to delay surgery for better blood sugar control needs to balance:
- Need for better vision
- Clear view of the fundus to manage retinopathy
- Patient’s ability to control diabetes with improved vision
Research shows better HbA1c levels before surgery lead to better vision improvement (r = -0.51), showing well-controlled diabetes helps achieve superior outcomes.
Functional vision vs cataract severity correlation
Doctors need to find out if poor vision comes from cataracts or underlying retinopathy in diabetic patients. Research shows visual acuity tests alone don’t give the full picture. Yes, it is wrong to base cataract surgery decisions only on visual acuity results.
Advanced retinopathy makes it harder to connect cataract severity with functional vision. Studies reveal 94.2% of diabetic patients see better three months after surgery, but improvement decreases as baseline retinopathy gets worse. Patient satisfaction drops from 82.4% in those without retinopathy to just 40% in those with proliferative diabetic retinopathy.
Patients need detailed counselling about realistic expectations. They should know that removing cataracts fixes lens cloudiness, but retinal problems might still limit their final vision.
Intraoperative Adjustments for Safer Outcomes
Cataract surgery for diabetic patients comes with unique challenges that need specific adjustments during operation to get the best results. A diabetic eye reacts differently to standard surgical methods, so surgeons must modify their techniques to ensure patient safety.
Managing poor pupil dilation in diabetic eyes
Many diabetic patients have trouble with proper pupil dilation, which makes removing cataracts more difficult. This happens because glycogen builds up in the iris pigment epithelium and diabetes can cause new blood vessels to grow. Research shows posterior capsule rupture happens almost six times more often when pupils don’t dilate well.
Doctors can take several approaches when diabetic eyes don’t dilate well:
- Pharmacological assistance: Intracameral agents like unpreserved lidocaine or diluted epinephrine help improve dilation in some diabetic eyes
- Mechanical devices: Iris hooks, pupil expansion rings (like Malyugin Ring), or similar devices are reliable ways to expand the pupil
- Surgical techniques: Viscodispersive agents help maintain space, though they might not last through the whole procedure
Doctors should avoid stretching the pupil in diabetic patients, especially those with active or regressed rubeosis iridis. These vessels might rupture and cause bleeding during surgery. Clinical studies show that 33.3% of small pupil cases need surgical management techniques.
Minimising phaco energy and fluidics
Diabetic cataracts often feel leathery and sticky, making standard phacoemulsification more challenging. These characteristics mean surgeons need to make specific adjustments to protect the corneal endothelium A full preoperative evaluation helps reduce cumulative dissipated energy (CDE). Patient age, cataract density, and diabetes all affect how much energy the procedure needs. Here’s how to keep energy use low:
Modern phaco machines with active-fluidics technology keep anterior chambers stable with minimal pressure changes. This stability lets surgeons use higher vacuum settings without post-occlusion surge and cuts down phacoemulsification time. Torsional or transversal ultrasound modes work better than traditional longitudinal energy delivery. They boost efficiency while using less energy. Doing phacoemulsification “in the bag” instead of the anterior chamber helps protect the endothelium.
Protecting the endothelium works best by coating it with a visco-dispersive agent or using a soft-shell technique. This involves layering visco-dispersive and cohesive agents in the anterior chamber.
Avoiding silicone IOLs in patients at risk of vitrectomy
IOL material choice matters a lot for diabetic patients. Doctors usually prefer acrylic IOLs for patients who might need vitrectomy for proliferative diabetic retinopathy later. Silicone IOLs raise concerns about future retinal surgery. If a diabetic patient needs vitrectomy with silicone oil tamponade, the oil might condense on silicone IOLs and cause vision problems. This interaction creates a risk that doctors must think about when choosing IOLs.
A 10-year study of diabetic patients getting vitrectomy showed interesting results. While doctors used silicone oil in 14% of diabetic eyes during vitrectomy, actual problems from silicone oil-silicone IOL interactions rarely happened. This suggests silicone IOLs might work for some diabetic patients, though doctors should still be careful. Hydrophobic acrylic single-piece foldable IOLs with a 6mm optic work well for diabetic patients. These lenses’ hydrophobic nature leads to fewer posterior capsular opacity cases—an important benefit since PCO happens more often in diabetic patients.
Postoperative Care and Monitoring in Diabetic Patients
Diabetic patients need specialised care and careful monitoring after cataract surgery to achieve the best visual results. Their eyes present unique challenges that require specific approaches to prevent complications and ensure proper healing.
Topical NSAIDs and steroids for inflammation control
Diabetic patients’ eyes are more prone to prolonged inflammatory responses, making inflammation control after surgery vital. A combination of topical steroids and nonsteroidal anti-inflammatory drugs (NSAIDs) serves as the life-blood of post-cataract care for diabetic patients. Research shows this combined approach works better than using steroids alone.
Topical NSAIDs play a vital role in lowering the risk of postoperative macular oedema (PME). Research shows diabetic patients who received additional topical NSAIDs had a 77.9% lower risk of developing PME at one month post-surgery. NSAIDs block cyclooxygenase (COX), which reduces pro-inflammatory prostaglandins that break down the blood-retinal barrier.
Prednisolone acetate eye drops remain essential but need careful monitoring in diabetic patients. Topical steroids can affect blood glucose levels even with minimal systemic absorption (≤2% of the applied dose). A typical postoperative regimen includes:
- Topical antibiotics (e.g., ciprofloxacin 0.3%) for 2-3 weeks
- Prednisolone acetate (0.12-1%) for 4 weeks
- NSAIDs (e.g., diclofenac sodium 0.1%) for 10 days to 2 months
OCT monitoring for macular oedema
Optical Coherence Tomography (OCT) has become essential in monitoring diabetic patients after cataract surgery. Simple phacoemulsification can increase central macular thickness in diabetic eyes. Studies reveal diabetic patients have a 22% incidence of macular oedema after cataract surgery.
OCT examination timing matters greatly. Central macular thickness usually increases right after surgery and peaks at 4-6 weeks postoperatively. Diabetic patients need:
- Baseline OCT before surgery
- Follow-up scans at 1 month and 3 months
- Extra monitoring at 6 weeks to spot late-developing macular oedema
Pre-existing diabetic retinopathy severity relates strongly to postoperative macular oedema. Patients with moderate to severe nonproliferative or proliferative diabetic retinopathy show substantially greater macular thickening (145μm at 1 month) compared to those without retinopathy (18μm).
Posterior capsular opacification and laser treatment
Posterior capsular opacification (PCO), also known as secondary cataract, is the most common long-term complication after cataract surgery. PCO affects up to 50% of patients within five years. Diabetic patients develop PCO more frequently and earlier than non-diabetic individuals.
Research shows PCO rates between diabetic and non-diabetic patients remained similar during the first year after surgery. However, diabetic patients’ PCO values increased substantially after 18 months. This is a big deal as it means that diabetic patients needed Nd:YAG laser capsulotomy treatment more often.
YAG laser capsulotomy offers a quick and usually painless solution. Ophthalmologists use a precisely focused laser to create a small opening in the clouded posterior capsule, which restores clear vision. This outpatient procedure:
- Takes approximately 5-10 minutes
- Requires pupil dilation before treatment
- Has minimal risk, though diabetic patients show slightly higher complication rates
Diabetic patients should get regular check-ups to evaluate PCO development, as early treatment prevents unnecessary vision loss.
Choosing the Right Intraocular Lens for Diabetics
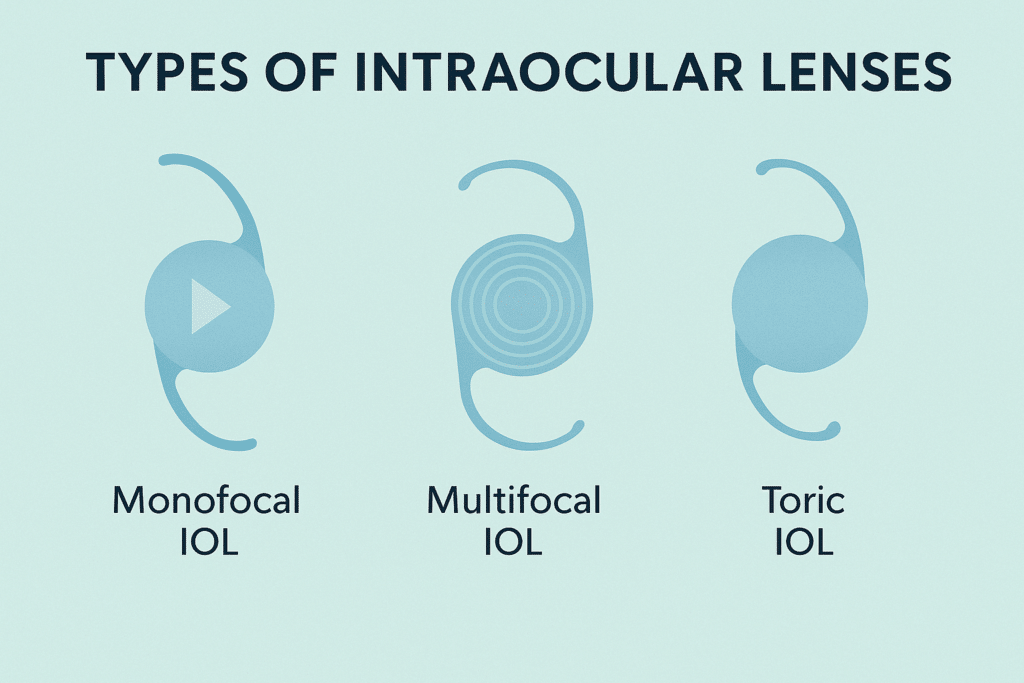
The choice of intraocular lens (IOL) is a vital decision for diabetic patients who need cataract surgery. Doctors must balance visual requirements with eye health because diabetes changes how eyes heal and respond to surgical procedures.
Monofocal IOLs and the need for reading glasses
Monofocal lenses stand out as the most dependable option for many diabetic patients. These lenses deliver sharp vision at one distance while maximising clarity. Standard lenses focus on just one distance—usually distance vision—which makes them eligible for insurance coverage. You’ll probably need reading glasses for close-up tasks like reading, using your smartphone, or working on your computer after getting monofocal IOLs.
Diabetic patients with astigmatism who skip toric correction might need glasses for both far and near vision. Monofocal IOLs give predictable results with minimal side effects. This becomes more important because diabetic patients’ healing patterns are nowhere near as predictable.
Why multifocal lenses may not suit diabetic retinopathy
Reduced dependence on glasses sounds appealing, but doctors rarely recommend multifocal IOLs to patients with diabetic retinopathy. These lenses divide light to create multiple focal points. The design can reduce contrast sensitivity even in healthy eyes. Diabetic retinopathy already affects visual quality, so adding a lens that decreases contrast could make vision worse.
Research shows multifocal lenses can substantially decrease vision quality in patients with macular oedema. Eye doctors stay cautious about suggesting multifocal IOLs if they spot any macular changes. Alternative options work better unless your diabetes stays very stable and well-controlled with minimal retinopathy.
Light Adjustable Lens (LAL) for post-op customisation
Light Adjustable Lens technology brings new hope to diabetic cataract patients. This lens, the first and only FDA-approved adjustable IOL, lets doctors adjust power after surgery. LAL offers flexibility through painless UV light treatments in the doctor’s office. This helps because diabetes can make healing patterns unpredictable.
Diabetic patients get these key benefits:
- Post-operative customisation after eye healing
- Better satisfaction from more accurate vision results
- Less need for glasses with custom vision correction
LAL technology helps diabetic patients whose healing might differ from expected outcomes by allowing adjustments that match individual needs.
How Precision Vision London Ensures Safe Cataract Surgery for Diabetics
Precision Vision London manages cataract surgery for diabetic patients through a precise protocol that addresses their unique challenges. Diabetic? Cataract surgery needs a tailored approach. Learn how Precision Vision London ensures safe, effective outcomes for every patient. The clinic acknowledges that diabetic individuals make up 20% of all cataract surgeries. This significant number requires care beyond standard procedures.
Advanced diagnostics for pre-surgical planning
Precision Vision London’s pre-surgical evaluations go beyond standard protocols. These evaluations have:
- Optical Coherence Tomography (OCT) and OCT angiography that identify subtle macular changes standard examinations often miss
- Detailed dilated fundus examinations that show retinopathy severity
- HbA1c assessment that shows glycemic control levels before surgery
- Corneal topography that identifies diabetic corneal changes affecting surgical planning
The clinic works with endocrinologists to optimise blood glucose control before surgery, following 10-year old protocols that minimise surgical risks.
Experienced surgeons trained in diabetic eye care
Precision Vision London’s surgical team specialises in diabetic eye care. They know that “complex patients do better when surgery is performed by a more experienced surgeon rather than a novice”. The surgeons use micro-incisional techniques that minimise trauma and help diabetic patients heal faster. They also apply refined phacoemulsification methods with minimal energy to protect the diabetic corneal endothelium.
Personalised IOL selection and postoperative follow-up
IOL selection plays a crucial role. The clinic prefers hydrophobic acrylic IOLs for diabetic patients who might need future retinal interventions. The team avoids silicone materials because they could complicate vitrectomy procedures needed for proliferative retinopathy management.
The postoperative care works hand in hand with careful lens selection and includes:
- Rigorous NSAIDs and steroid protocols that prevent macular oedema
- Regular OCT monitoring that catches early signs of complications
- Extended follow-up schedule compared to non-diabetic patients
Advanced diagnostics, specialised surgical expertise, and customised postoperative care help Precision Vision London achieve optimal outcomes for diabetic cataract patients.
Conclusion
Cataract surgery for diabetic patients needs specialised care throughout the whole ordeal. Diabetes speeds up cataract formation by a lot and raises the risk of complications during and after surgery. A detailed preoperative evaluation becomes crucial, with a full picture of retinopathy and careful blood glucose control checks.
Diabetic patients need specific adjustments during the surgery. The surgeon must handle poor pupil dilation, reduce phacoemulsification energy, and pick the right intraocular lens materials. After surgery, the care must stay precise with close monitoring of inflammation and regular OCT scans for macular oedema.
Diabetic patients can achieve excellent vision despite their unique challenges with the right specialised care. Precision Vision London’s expertise comes from advanced diagnostics, surgeons trained in diabetic eye care, and customised follow-up protocols. The clinic’s steadfast dedication to understanding diabetes and eye health will give a safe, effective treatment path.
Your surgical outcome depends heavily on getting care from specialists who understand your specific needs. Proper preoperative checks, precise surgical technique, and careful post-surgery monitoring are the foundations of successful vision restoration. Your vision deserves this level of specialised attention and expertise.
FAQs
Q1. What special precautions are taken for diabetic patients before cataract surgery? Diabetic patients undergo comprehensive eye examinations, including retinopathy assessment and blood glucose level checks. They may be advised to optimise their blood sugar control and are often scheduled for surgery early in the day.
Q2. How does cataract surgery differ for diabetic patients compared to non-diabetics? Cataract surgery for diabetics requires extra care due to increased risks. Surgeons use specialised techniques to manage poor pupil dilation, minimise phacoemulsification energy, and select appropriate intraocular lenses to accommodate potential future retinal treatments.
Q3. What are the potential complications of cataract surgery for diabetic patients? Diabetic patients may face a higher risk of macular oedema, progressive retinopathy, and limited vision improvement post-surgery. The procedure can put additional stress on eyes with pre-existing diabetic eye disease.
Q4. Are multifocal intraocular lenses recommended for diabetic patients? Multifocal lenses are typically not recommended for patients with diabetic retinopathy. These lenses can compromise contrast sensitivity, which may further deteriorate vision quality in diabetic eyes that already have compromised retinal function.
Q5. How important is postoperative care for diabetic cataract patients? Postoperative care is crucial for diabetic patients. It includes rigorous use of anti-inflammatory medications, regular OCT monitoring for macular oedema, and an extended follow-up schedule compared to non-diabetic patients to detect and manage any complications early.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

