Research shows that corneal cross-linking works to stop keratoconus from getting worse for most patients. This treatment brings new hope to 1 in 500 people who live with this condition. Your vision’s future might worry you after a keratoconus diagnosis, but this breakthrough treatment can improve your outlook by a lot.
Scientists haven’t found a cure for keratoconus yet, but corneal cross-linking has revolutionised patient care. The procedure boasts impressive success rates that stabilise the cornea and can enhance both its shape and visual function. Patients often avoid more complex surgeries like corneal transplants. This becomes crucial since 83% of corneal transplants start to fail after 23 years.
Our team at Precision Vision London knows your worries about keratoconus treatments. This piece cuts through myths and facts to give you clear answers about corneal cross-linking. You’ll learn about its success rates and what to expect from our advanced treatment methods. We’re here to help you protect your vision’s future with the right information and choices.

What is Corneal Cross Linking?
Corneal cross linking represents a breakthrough treatment for progressive corneal disorders. Let me explain what this treatment involves and how it works.
Understanding the corneal structure
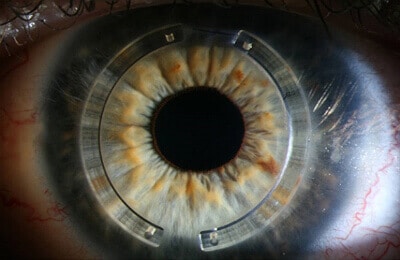
Your eye’s clear front window is the cornea—a dome-shaped transparent covering that handles most of your eye’s focusing power. The cornea contains collagen fibres that form a specific pattern to maintain its shape and strength. When someone has keratoconus, this normally round structure becomes weaker over time. It gets thinner and bulges outward like a cone. This distortion substantially disrupts vision because the cornea cannot focus light properly onto the retina.
Corneal cross linking definition and purpose
Corneal cross linking (CXL) strengthens the cornea through new bonds between collagen fibres. We used ultraviolet light and vitamin B2 (riboflavin) to stiffen the cornea and stop keratoconus from getting worse. The riboflavin absorbs UV light and creates a photochemical reaction inside the corneal tissue. This reaction helps form extra bonds between collagen fibres and improves corneal stability. In fact, CXL copies the natural age-related stiffening of the cornea, which explains why keratoconus usually stabilises in patients after middle age. The treatment has achieved a soaring win with more than 90% success rate in preventing keratoconus progression.
How the cross linking operation works
Doctors perform the cross linking operation as an outpatient procedure that takes less than 30 minutes. The process starts with numbing your eye using anaesthetic drops. The ophthalmologist then gently removes or loosens the cornea’s thin outer layer (epithelium) so the medication can penetrate deeper. Here’s what happens next:
- The cornea receives riboflavin (vitamin B2) drops every few minutes for about 10-30 minutes until it’s fully saturated
- A focused UV light beam targets the cornea for approximately 8-30 minutes and activates the riboflavin
- This light activation creates new bonds between collagen fibres
- A soft “bandage” contact lens helps your eye heal
The riboflavin serves two purposes during the procedure—it enables the cross-linking reaction and protects deeper eye structures from UV exposure. Precision Vision London’s team conducts this procedure with careful attention to safety and comfort through advanced technology and expert surgical techniques.
8 Common Myths About Corneal Cross Linking
Several myths about corneal cross linking continue to circulate, even though this procedure works well. Our team at Precision Vision London wants you to have accurate information to make smart choices about your eye health.
Myth 1: Cross linking is painful
The procedure doesn’t hurt because we use anaesthetic eye drops. Patients might feel some discomfort for 24-48 hours afterward, but prescribed medication manages this well. Most discomfort peaks during the first night and gets better gradually.
Myth 2: It only works in advanced keratoconus
In stark comparison to this belief, treating keratoconus early leads to better results. The treatment works best in earlier stages and prevents the condition from getting worse. Young patients who wait too long risk their condition progressing quickly.

Myth 3: It cures keratoconus completely
This treatment stabilises keratoconus but doesn’t cure it. The procedure halts progression in more than 90% of cases. In spite of that, you’ll need glasses or contact lenses afterward because CXL can’t reverse existing corneal changes.
Myth 4: Contact lenses are enough
Contact lenses help correct vision but can’t stop keratoconus from getting worse. The treatment addresses the weak corneal structure, while lenses just help you see better without affecting how the disease progresses.
Myth 5: It’s not covered by insurance
Most insurance plans now cover this treatment. It has become accessible to more people as a standard treatment rather than an experimental procedure.
Myth 6: It’s a one-time permanent fix
One treatment is enough for most people. About 7-8% of patients might see their condition progress even after treatment. So some patients, especially children, might need a second procedure.
Myth 7: It’s unsafe or experimental
Long-term data proves that corneal cross linking is remarkably safe. Research shows keratoconus remained stable in 99.2% of eyes three years after treatment. Serious complications happen in less than 3% of cases.
Myth 8: It’s only for young patients
The treatment helps patients from age 8 to mid-40s. More research shows that older people can experience significant progression too, even though younger patients’ conditions typically progress faster.
How Effective is Corneal Cross Linking for Keratoconus?
Research shows corneal cross linking works remarkably well to manage keratoconus.
Slowing or halting disease progression
Clinical studies show corneal cross linking stops keratoconus progression in more than 90% of treated cases. The largest longitudinal study up to 10 years confirms this stabilising effect stays consistent. The results are impressive – 99.2% of patients showed no further progression after three years of monitoring.
Improving corneal stability and shape
Corneal cross linking does more than just stop progression. Many patients’ corneal shape gets better after treatment. Their maximum keratometry (Kmax) drops by about 1.30 diopters, which shows the cornea’s conical shape flattens out. This structural improvement helps patients maintain stable vision as they recover.
Reducing the need for corneal implant or transplant
The treatment has cut down the need for corneal transplants. Before cross linking became available, about 20% of keratoconus patients needed transplantation. The UK has seen a 25-50% drop in corneal transplants for keratoconus since doctors started using cross linking.
UK-based clinical outcomes and success rates
The National Institute for Health and Care Excellence (NICE) recognised corneal cross linking as safe and effective to manage keratoconus in 2013. Precision Vision London provides proven corneal cross-linking that stabilises vision and protects future sight. UK clinical data shows this treatment stays affordable for at least 14 years after the procedure.
What to Expect at Precision Vision London
Your choice of clinic for corneal cross linking can shape your treatment results and experience. Precision Vision London’s trained patient coordinators will guide you from your first contact.
Personalised consultation and diagnostics
The team will use state-of-the-art technology to assess your corneal condition. Precision Vision London’s team knows that determining your suitability is a vital part of providing treatments that match your visual and lifestyle needs. Their detailed pre-treatment assessment will give you a personalised treatment plan designed for the best possible outcomes. Book your consultation today for expert advice and treatment options.
Advanced technology and safety protocols
You can choose between epithelium-off and epithelium-on procedures based on your specific needs. Patients receive the latest cross-linking techniques with careful attention to safety. Precision Vision London has earned a 4.97/5 rating from 166 verified reviews, making it London’s top-rated corneal cross linking clinic.
Expert surgeons and aftercare support
Dr. CT Pillai, Medical Director and lead surgeon, holds dual fellowships in corneal and refractive surgery—a difference few specialists in the country can claim. He and his team bring over 30 years of ophthalmic surgical experience. Your aftercare starts right in the recovery room, and a specialist nurse will examine you before discharge. You’ll also have access to the country’s largest independent optometrist network, which lets you get follow-up care closer to home.
Conclusion
Research strongly shows that corneal cross linking has revolutionised treatment options for keratoconus patients. This piece explores how the procedure stops disease progression in over 90% of cases and improves corneal stability. Cross linking doesn’t cure the condition completely, but it helps preserve your vision and prevents your corneal health from getting worse.
Time has cleared up many myths about this treatment. The procedure causes minimal discomfort, shows best results with early intervention, and years of clinical data prove its safety. The dramatic drop in corneal transplant rates across the UK proves its effectiveness as a primary treatment choice.
Your experience with keratoconus can be managed with proper care and treatment. Facts should guide your treatment decisions, not fear. We provide proven corneal cross-linking at Precision Vision London to stabilise your vision and safeguard your eyesight. Expert advice and treatment options await you at your consultation.
Getting diagnosed doesn’t mean facing an uncertain future. Dr. CT Pillai and our expert surgical team use cutting-edge diagnostic technology and create personalised treatment plans that address your specific visual needs. This straightforward outpatient procedure gives you long-term stability, and you can resume normal activities within days.
Taking early action remains your best defence against keratoconus progression. You might still need glasses or contact lenses afterward, but your stabilised vision will give you peace of mind for years. Today’s decision to get corneal cross linking could protect your eyesight for tomorrow.
Key Takeaways
Understanding the facts about corneal cross linking can help you make informed decisions about keratoconus treatment and protect your vision for the future.
- Corneal cross linking successfully halts keratoconus progression in over 90% of cases, preventing further vision deterioration without being a complete cure
- Early intervention delivers better outcomes than waiting for advanced stages, making prompt treatment crucial for optimal results
- The procedure is safe, minimally invasive, and typically covered by insurance, with serious complications occurring in fewer than 3% of cases
- Cross linking has reduced UK corneal transplant rates by 25-50%, offering a less invasive alternative to major surgery
- Most patients experience only mild discomfort for 24-48 hours post-procedure, with the treatment taking less than 30 minutes as an outpatient procedure
The evidence clearly demonstrates that corneal cross linking represents a transformative treatment option that can stabilise your corneal condition and preserve your quality of life for years to come.
FAQs
Q1. Is corneal cross-linking painful? The procedure itself is painless due to anaesthetic eye drops. Some discomfort may occur for 24-48 hours afterwards, which can be managed with prescribed medication. The peak discomfort typically occurs during the first night and gradually improves.
Q2. Can corneal cross-linking cure keratoconus completely? Corneal cross-linking is not a cure but rather a stabilisation treatment. It halts progression in more than 90% of cases but does not reverse existing corneal changes. Patients will still require vision correction with glasses or contact lenses after the procedure.
Q3. At what stage of keratoconus is cross-linking most effective? Early intervention with corneal cross-linking delivers better outcomes. The procedure is often more beneficial in earlier stages, preventing further progression rather than waiting until the condition worsens. Delaying treatment can result in rapid progression, particularly in younger patients.
Q4. How long does the corneal cross-linking procedure take? The corneal cross-linking operation is performed as an outpatient procedure that typically takes less than 30 minutes. This includes the application of riboflavin drops and exposure to UV light to activate the cross-linking process.
Q5. What is the success rate of corneal cross-linking for keratoconus? Clinical studies demonstrate that corneal cross-linking successfully halts keratoconus progression in over 90% of treated cases. Long-term studies spanning up to 10 years verify that this stabilisation effect remains consistent over time.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

