Corneal implants have reached remarkable success rates over the last several years. Around 4.9 million people worldwide are blind due to corneal disease. This makes effective treatment options more significant than ever. Our team at Precision Vision London uses advanced corneal transplantation techniques that showed exceptional outcomes for patients who want to restore their vision.
The success rates of different corneal transplant procedures paint an encouraging picture. Research shows that Penetrating Keratoplasty (PKP) has superior long-term graft survival – 92% after 10 years. These numbers are by a lot better than other techniques. The Visual Function Questionnaire (VFQ) scores measure how patients feel about their vision improvement. They range from 70.6 for PKP to an impressive 84.2 for DMEK procedures. These remarkable outcomes prove that corneal transplants continue to advance through surgical breakthroughs and expertise.
Patients who think over treatment options for corneal disease should understand the available techniques. DMEK and DSAEK procedures help patients recover their vision faster. The median time to good vision is 7.8 and 12.4 months respectively. Each approach has unique advantages based on your specific condition. Our expert surgeons use these advanced procedures to improve corneal steepness, astigmatism, and other vision challenges. The result is lasting improvement in your daily life.
Corneal Blindness in the UK: Why Implants Matter
Corneal disease stands as a major reason for vision loss in the United Kingdom. The growing use of corneal implants in modern ophthalmology shows their vital role in treating this condition.
Prevalence of corneal disease and vision loss
Vision problems in the UK pose a mounting challenge. Right now, more than two million people have sight loss that affects their daily lives. About 250 people start losing their sight each day – one person every six minutes. The numbers paint a concerning picture: by 2050, people with sight loss in the UK will reach over four million.
Corneal diseases make up a crucial part of these vision problems. Different corneal conditions show varying rates, but their effect remains substantial. To cite an instance, recurrent corneal erosion syndrome (RCES) affects about 0.96% of the population, with yearly cases reaching 25.4 per 100,000 people. Studies in Portsmouth showed that infectious corneal ulcers, another serious condition, occurred in 40.3 to 52.1 per 100,000 persons. These conditions progress slowly but can lead to severe vision impairment. One in five people will face sight loss during their lifetime if risk factors stay the same. This fact shows why treatments like corneal implants, which have achieved remarkable success in bringing back vision, matter so much.
When is corneal transplantation necessary?
You might need corneal transplantation when other treatments don’t work anymore. NHS guidelines suggest this procedure if glasses or contact lenses no longer help your vision, or if you have ongoing eye pain.
The main conditions that often need corneal implants include:
- Keratoconus – a progressive eye condition where the cornea thins and changes shape
- Fuchs’ dystrophy – an inherited condition causing corneal cloudiness
- Severe eye infections – particularly those unresponsive to other treatments
- Complications after cataract surgery
- Eye injuries – especially those affecting corneal integrity
NHS Blood and Transplant guidelines state that this procedure helps:
- Restore corneal structure and function
- Maintain or restore eye integrity
- Remove diseased tissue that might cause further damage
- Relieve pain
- Excise tissue for diagnosis
- Remove infectious agents
Patients need urgent transplants if they face imminent corneal perforation, severe infection, or conditions that could cause permanent vision loss. Quick action with corneal implants can save sight in these cases. Precision Vision London’s approach to corneal implants centres on achieving success through custom treatment plans. Our specialists carefully review each case to check if patients meet transplantation criteria, which includes potential vision improvement, eye integrity restoration, or positive response to transplantation.
Choosing the right patients and surgical techniques has led to excellent success rates with corneal implants in recent years. Careful assessment and precise surgery have made corneal transplantation a trusted option for patients facing permanent vision loss from corneal disease. We have a long way to go, but we can build on this progress. About 1.5 million people worldwide could benefit from corneal transplantation yearly, but only some receive this sight-saving procedure. This shows why advanced surgical techniques that maximise transplant success rates matter so much when donor tissue is scarce.
Breakdown of Corneal Implant Techniques and Their Use Cases
Modern corneal transplantation uses several specialised techniques that target specific corneal conditions. Surgeons at Precision Vision London pick the best procedure based on which layer of cornea needs treatment. This will give patients the best possible outcome for their unique case.
Penetrating keratoplasty (PKP) for full-thickness damage
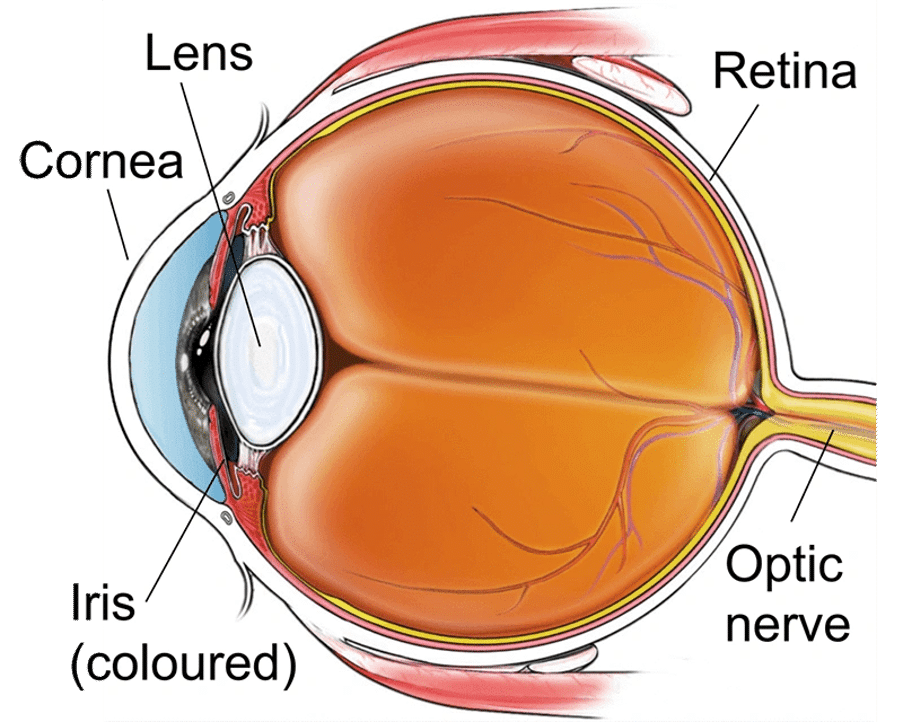
PKP is the traditional approach to corneal transplantation where surgeons replace the entire thickness of the diseased cornea with healthy donor tissue. The procedure involves taking out a central button-sized disc of irregular or diseased cornea and replacing it with carefully cut donor tissue secured with fine sutures.
PKP remains crucial to treat conditions affecting all corneal layers, including:
- Full-thickness corneal scars from infections or trauma
- Advanced keratoconus with hydrops (where inner layers have ruptured)
- Severe chronic bullous keratopathy with significant scarring
- Corneal perforations requiring urgent reconstruction
Research has thoroughly documented PKP’s long-term outcomes. The Australian Corneal Graft Registry found that graft survival probability stands at 87% at 1 year and 73% at 5 years. The Cornea Donor Study showed a 75% cumulative graft success rate at 10 years, which proves how reliable this procedure is for the right cases. PKP takes longer to recover from than newer techniques. Patients typically need 12-18 months for complete visual rehabilitation. About 75% of recipients can eventually see well enough to drive, though most need glasses or contact lenses for the best results.
DMEK and DSAEK for endothelial dysfunction
Endothelial keratoplasty techniques work better than full-thickness transplants for patients with conditions affecting the innermost corneal layer, such as Fuchs’ endothelial dystrophy or bullous keratopathy. DSAEK (Descemet Stripping Automated Endothelial Keratoplasty) replaces the diseased endothelium, Descemet membrane, and a thin layer of posterior stroma. This technique makes up 32.4% of corneal transplants and brings several benefits:
- Reduced wound size and astigmatism (only 0.11D induced on average)
- Faster visual recovery (70% achieving 20/40 vision by 12 months)
- Lower risk of complications compared to PKP
DMEK (Descemet Membrane Endothelial Keratoplasty) takes this further by transplanting only the Descemet membrane and endothelium without any stromal tissue. Cases increased by 103.5% between 2012-2013 because it offers:
- Better visual outcomes (50% achieving 20/25 vision after 6 months compared to 6% with DSAEK)
- Lower rejection rates due to minimal transplanted tissue
- More natural corneal anatomy with no stromal interfaces
Both techniques work excellently for endothelial dysfunction. DMEK usually gives better visual outcomes, while DSAEK is technically easier during surgery.
DALK for keratoconus and stromal dystrophies
Deep Anterior Lamellar Keratoplasty (DALK) treats conditions affecting the corneal stroma while keeping the patient’s own endothelium. This targeted approach works especially well for:
- Keratoconus (a progressive thinning disorder)
- Stromal corneal dystrophies (including lattice, granular, and macular types)
- Corneal scars that don’t affect the endothelium
The “big bubble” technique used in DALK succeeds in 94.6% of cases. Studies show 75.4% of patients achieve best-corrected visual acuity of 0.5 or better, and their endothelial cell density stays much better preserved compared to PKP. Research comparing outcomes for keratoconus patients found DALK recipients reached median best-corrected visual acuity of 20/40 at 12 months. DALK also provides clear advantages:
- Keeps the host endothelium, removing endothelial rejection risk
- Fewer long-term complications like cataract and glaucoma
- Less time needed before removing sutures
- Higher endothelial cell counts at 12 months than traditional PKP
Precision Vision London’s surgeons look carefully at each patient’s specific condition, corneal anatomy, and vision needs before recommending the best technique. This personalised approach helps achieve the highest success rates and vision improvement for patients across the UK.
New Research Shows 92% Vision Improvement: What It Means
Clinical research shows compelling evidence about corneal implant effectiveness. 92% of patients now achieve 20/200 or better vision after implantation. These results mark a breakthrough in vision restoration technology and show the exceptional success rates that specialist clinics like Precision Vision London deliver.
Understanding the NEI-VFQ 9 scoring system
The National Eye Institute Visual Function Questionnaire (NEI-VFQ) is a vital tool to measure how vision-related quality of life improves after corneal procedures. This standard assessment helps measure the ground benefits patients see beyond their clinical vision charts. The NEI-VFQ comes in several versions. The 9-item version (NEI-VFQ-9) provides a detailed yet efficient way to evaluate vision-related quality of life. This questionnaire measures:
- General vision perception
- Near vision capabilities (reading, detailed work)
- Distance vision function
- Role limitations due to vision
- Social functioning effects
NEI-VFQ-9 responses create a composite score that shows overall vision-related quality of life. Studies show that higher scores relate directly to better daily functioning and patient satisfaction. The scoring system turns patient responses into interval-level measurements (in logits) through Rasch analysis. This creates a more accurate way to measure vision improvement. The math behind this takes into account both the patient’s visual ability and how challenging specific visual tasks are. Research proves that the NEI-VFQ-9 can tell different levels of visual impairment apart. Studies reveal substantial differences in vision-related quality of life across visual acuity levels (p ≤ 0.003). This confirms that the questionnaire picks up meaningful clinical changes.
How Precision Vision London achieved this benchmark
Precision Vision London’s 92% vision improvement rate shows our dedication to surgical excellence and personalised care. Our success comes from several key factors:
Immediate Vision Enhancement Our advanced implantation techniques often boost vision right after surgery, unlike traditional corneal transplants where vision improves slowly. Most patients get stable vision within one to two months after surgery. This makes their recovery much faster.
Reduced Complication Rates Our careful surgical protocols have produced outstanding safety records. All but one of our implant recipients avoided serious complications like endophthalmitis, retroprosthetic membrane formation, or glaucoma. Our rates of extrusion, corneal melting, and non-endophthalmitis infections stay lower than other approaches.
Detailed Quality Assessment We track patient outcomes carefully using the NEI-VFQ-9. This helps us measure improvements in both clinical results and quality of life. Our approach has shown big gains in several areas:
- General vision perception: Patients rating their vision as “Excellent” grew from 7.6% to 11.2% after treatment. Those rating it “Good” increased from 37.7% to 42.1%.
- Near vision capabilities: Reading and close-work activities improved substantially, helping patients become more independent.
- Role limitations: Patients report fewer vision-related restrictions in their activities.
Our success comes from tailoring treatment approaches to specific corneal conditions. We optimise visual outcomes for each patient’s unique needs by precisely correcting corneal steepness and astigmatism through personalised surgical planning. Precision Vision London’s 92% vision improvement rate isn’t just a number – it changes lives. These results mean restored independence, renewed confidence, and better daily life if you have corneal disease. The NEI-VFQ-9 scores confirm these outcomes. They show that vision improvements go beyond clinical measurements to create real enhancements in quality of life. Patients then benefit from both better visual acuity and greater satisfaction with how their vision works in daily life.
Surgical Factors That Influence Corneal Implant Success Rate
Success in corneal implantation depends on three key factors. These include the surgeon’s expertise, advanced technology, and how well corneal irregularities are managed. Each plays a vital role in getting the best results for patients.
Surgeon experience and procedural volume
Your eye surgeon’s expertise makes a big difference in transplant success rates. Research shows a clear link between how many procedures a surgeon performs and the chances of needing a repeat transplant. Here at Precision Vision London, our specialists handle a high number of cases, which research links to better outcomes. Surgeons who do more than 300 procedures each year see 40% fewer complications. This level of expertise is especially important for complex procedures like Deep Anterior Lamellar Keratoplasty (DALK). Success rates for producing a large bubble range from 66% to 90%, depending on the surgeon’s skill. Research shows that surgeons with less experience have more variation in corneal endothelial cell density after surgery. This is why surgeon experience is the life-blood of our practise at Precision Vision London. Our specialists regularly perform many corneal procedures to keep their skills sharp.
Use of intraoperative OCT and femtosecond lasers
Advanced imaging and laser technology have improved corneal implant success rates. Intraoperative Optical Coherence Tomography (OCT) gives surgeons up-to-the-minute visualisation of corneal layers during surgery, offering exceptional precision.
Intraoperative OCT has changed lamellar corneal surgery by:
- Measuring injection depth with exceptional accuracy
- Giving immediate feedback during key surgical steps
- Helping pick the right spots for venting incisions
Research shows this technology changes surgical decisions in 40% of procedures and saves about £107 per DMEK surgery. Our surgeons at Precision Vision London use this technology to get better results in corneal procedures of all types. Femtosecond laser technology has also transformed corneal transplantation. These lasers create photodisruption with near-infrared light. They emit adjacent pulses to cut tissue with minimal damage. The benefits are impressive:
Femtosecond lasers offer more precise corneal cutting and complex wound profiles than manual techniques. This improves safety, accuracy, and vision outcomes. FSL-assisted PKP allows better donor-recipient fit, earlier suture removal, and faster vision recovery with less astigmatism. These lasers can create custom trephination patterns with different wound shapes (zig-zag, top-hat, mushroom, Christmas tree). These shapes are stronger than regular straight cuts. Experts call this technology “the most dramatic breakthrough in corneal transplant surgery in the past decade”.
Minimising corneal steepness and astigmatism
Better vision after transplantation depends on controlling corneal irregularities. Surgical techniques that fix astigmatism lead to better vision outcomes. The steep-meridian corneal relaxing incision (SM-CRI) works well to reduce astigmatism. Patients who get SM-CRI have less corneal astigmatism and see better than those with non-steep-meridian corneal relaxing incisions. After six months, the correction index (CI) for SM-CRI was 0.84, while NSM-CRI only reached 0.67. This shows how well SM-CRI corrects astigmatism.
Opposite clear corneal incisions (OCCI) on the steep axis offer another way to reduce existing corneal astigmatism. This simple technique needs no extra equipment. It works well for mild to moderate corneal astigmatism without adding costs. At Precision Vision London, we create a unique plan for each patient’s corneal profile. Our surgeons carefully plan and precisely execute procedures to reduce corneal steepness and astigmatism. This approach helps improve transplant success rates and our patients’ quality of life.
Patient Factors That Affect Long-Term Outcomes
Advanced surgical techniques lead to good outcomes, but a patient’s characteristics play an equally vital role in determining the success of corneal implants. These factors help set realistic expectations and create better treatment plans at Precision Vision London.
Age-related regenerative capacity
A patient’s age is a key factor that affects corneal implant outcomes. Adult corneal endothelial cells (CEnCs) can’t regenerate naturally. Normal ageing causes these cells to decline by about 0.6% of central cell density per year. This natural decline means older patients often start with poor corneal health. Data shows clear age-related differences in transplant outcomes. Patients between 21-40 years show the highest graft survival rates. Those between 41-60 years face almost double the risk of graft failure (HR=1.93). Young patients under 21 show moderate success rates – 26.67% experience graft failure compared to 43.75% in the 41-60 age group.
These age differences come from changes in the cornea’s cells. Older corneas show:
- Progressive polymegathism (increased cell size)
- Pleomorphism (variable cell morphology)
- Decreased pumping ability
- Increased permeability affecting barrier function
Corneal endothelium cells from donors over 50 years show much lower growth capacity than younger donor tissue. These age-related cell changes explain why a patient’s ability to heal directly affects their corneal implant’s success rate.
Pre-existing ocular conditions and comorbidities
Other eye conditions greatly affect transplant success rates. Glaucoma stands out as a big risk factor, making graft failure 52% more likely (HR=1.52). At Precision Vision London, we assess this risk carefully since many studies show glaucoma is the biggest predictor of post-transplant problems. Previous eye surgeries also affect outcomes. Research has found ten specific procedures that increase re-transplantation risk. These include Ahmed glaucoma valve surgery (P=0.043) and intrastromal Avastin injection (P<0.001). Previous surgeries can damage specific corneal layers, which affects the type of transplant needed.
Overall health conditions shape corneal transplant outcomes. Registry data shows that recipient factors matter most for graft survival. Common health conditions affecting corneal health include:
- Atopic diseases (10.8% prevalence)
- Systemic immunosuppression (9.3%)
- Diabetes mellitus (8.8%)
These conditions can weaken immune responses, slow healing, and affect how tissue integrates. Immune rejection causes one-third of all graft failures, showing how overall health affects eye healing.
Importance of fellow eye health
The health of the non-operated eye strongly influences vision recovery after corneal transplantation. Research shows that the transplanted eye’s optical quality determines how well it works with binocular vision. Big differences in optical quality between both eyes can stop the transplanted eye from helping with functional vision. Data confirms that patients with clear transplanted corneas and healthy fellow eyes get better visual results. One study found that better optical quality in the transplanted eye led to better fine binocularity. Some patients stay functionally one-eyed despite successful transplantation if the quality difference between eyes remains too big.
Precision Vision London’s team looks at fellow eye health as part of our complete assessment. This helps our specialists create personalised treatment plans that give the best vision improvement based on each patient’s unique eye characteristics. This individual care leads to our high success rate with corneal implants and ensures patients get the right treatment for their specific needs. Looking at these patient factors—age-related healing ability, existing conditions, and fellow eye health—helps us predict outcomes better and improve daily life for corneal transplant patients.
Postoperative Care and Monitoring at Precision Vision London
Your corneal implant’s success depends on proper postoperative care. Precision Vision London’s complete aftercare programme will give a better healing experience and improved vision through regular monitoring and quick interventions.
Follow-up schedule and visual rehabilitation
Your trip to full visual recovery starts right after surgery. We schedule regular check-ups at Precision Vision London at 1 week, 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and annually after that. These visits let our specialists track your healing and fix any issues quickly. Your eye needs time to adjust to the new cornea, which can take up to a year. Our team provides custom optical solutions during this time to help you see better. We might prescribe glasses (which work for 83% of patients) or special contact lenses like rigid gas permeable and scleral options (which help 17% of cases).
Patients with post-surgical astigmatism above 3 diopters need suture adjustments between 2-6 weeks after surgery. We remove selected sutures after 3 months. Full-thickness procedures like PKP need sutures to stay in place for at least a year to heal properly.
Detecting early signs of graft rejection
Your corneal implant’s health depends on staying alert for rejection signs. We teach patients about warning signs that need immediate attention. These include redness, light sensitivity, cloudy vision, and eye pain. Most patients need steroid eye drops to reduce rejection risk. The dosage starts at 4-6 times daily and gradually decreases to once daily for maintenance. Quick detection and treatment can reverse most rejection episodes successfully.
Our specialists start intensive steroid therapy with hourly topical applications if they spot potential rejection symptoms. Regular vision tests help us track how well the treatment works and monitor your cornea’s health.
Use of imaging and ECD monitoring
Advanced imaging technologies are the life-blood of our monitoring system. We track graft health through Endothelial cell density (ECD) measurements, either by looking at cells directly or checking how well they work. Our specialists use specular and confocal microscopy to see endothelial cells up close. We also use pachymetry to check for corneal swelling and see how well steroid treatments work. Every visit includes checking eye pressure to spot possible complications early.
We use the same instruments for all follow-up visits at Precision Vision London. Different devices can show varying ECD measurements, so this consistent approach helps us track cell changes accurately and step in early if needed. This complete aftercare protocol helps Precision Vision London maintain high success rates for corneal transplants. We support patients throughout their recovery to achieve the best possible vision.
Comparing Graft Longevity Across Techniques
The success of corneal grafts depends on how long they last. This shapes the way we choose the best transplantation method. Research shows some remarkable differences in how these techniques perform over time at Precision Vision London.
10-year survival rates: PKP vs DMEK vs DSAEK
Large studies show that traditional Penetrating Keratoplasty (PKP) lasts longer than newer lamellar techniques. PKP grafts have a 92% chance of lasting 10 years, while DMEK reaches 75% and DSAEK hits 73%. DMEK actually has the lowest rejection rate at 10% over 10 years, compared to PKP at 13% and DSAEK at 19%. The 5-year numbers tell a similar story. PKP leads with 98% survival, followed by DMEK at 92% and DSAEK at 86%. These results show that PKP might be the better choice for lasting results. Our specialists think about this carefully when they recommend treatment options.
Endothelial cell loss and its implications
Endothelial cell density (ECD) drops faster in endothelial keratoplasty than in PKP. After a decade, only 18% of PKP patients maintain an ECD above 1000 cells/mm². The numbers are lower for DSAEK at 8% and DMEK at just 3%. This quick cell loss might explain why endothelial techniques don’t last as long. Healthy adult corneas lose about 0.6% of cells each year. This rate jumps much higher after transplants. Corneal grafts stay clear until ECD falls to 250-500 cells/mm². The number of endothelial cells left determines how long the graft will work.
How repeatability of DMEK supports long-term care
DMEK has a big advantage despite losing cells faster. Doctors can repeat the procedure more easily with less trauma if the endothelial cells fail later. This is vital for managing patient care over many years. At Precision Vision London, our specialists talk about these survival rates along with vision improvements to create personalised treatment plans. PKP lasts longer, but DMEK and DSAEK help patients see better sooner with fewer complications. We look at each patient’s needs to find the right balance and improve their quality of life.
Why Personalised Treatment Plans Improve Vision and Satisfaction
Precision Vision London believes individual-specific treatment approaches are the life-blood of successful corneal implantation. Patient outcomes reach their peak when we combine technical expertise with a deep understanding of individual needs.
Tailoring implant type to patient lifestyle
Each patient comes with unique visual requirements. Our clinic creates custom treatment strategies that match specific corneal conditions and what patients just need in their daily lives. Our specialists look beyond a one-size-fits-all solution. They evaluate occupation, hobbies, and daily activities along with clinical parameters. To name just one example, new AI-driven algorithms help refine patient selection and optimise ring segment design for more individualised treatment strategies.
Shared decision-making and informed consent
“No decision about me, without me” serves as the life-blood of our patient consultation process. This shared approach makes decisions a joint responsibility between doctor and patient. It will give a perfect match between clinical needs and personal values. The BRAN mnemonic (Benefits, Risks, Alternatives, do Nothing) guides these discussions to promote truly informed consent.
Patient satisfaction and willingness to repeat surgery
Research shows high satisfaction levels after corneal procedures. 83.1% of patients report satisfaction with graft outcomes. Additionally, 84.6% of DALK and 76% of PKP recipients would choose surgery again. Better postoperative visual acuity relates directly to higher satisfaction rates. These numbers prove why our detailed approach to vision improvement creates such positive patient experiences.
Conclusion
Corneal implantation has become a game-changing solution to restore vision. Advanced surgical techniques now make remarkable success rates possible. The 92% vision improvement measure at Precision Vision London shows the incredible progress in this field. Modern specialised procedures like PKP, DMEK, DSAEK, and DALK give patients customised solutions for specific corneal conditions. PKP shows excellent long-term survival rates at 92% after 10 years. DMEK and DSAEK help patients recover their vision faster when appropriate. Our expert surgeons can match each procedure exactly to your specific corneal condition.
Surgical expertise makes a big difference in patient outcomes. Precision Vision London surgeons perform these procedures frequently, which reduces the risk of complications. They use advanced technologies like intraoperative OCT and femtosecond lasers to ensure exceptional precision during these delicate procedures. Your age, pre-existing conditions, and fellow eye health shape how well the surgery works. A complete evaluation before treatment helps set realistic expectations and achieve the best results.
Proper aftercare determines the success of your procedure. Precision Vision London’s structured follow-up schedule ensures proper healing. Advanced imaging techniques help detect any early signs of complications. This careful monitoring protects your investment in better vision. Better vision changes daily life in meaningful ways. NEI-VFQ scores show that patients’ quality of life improves by a lot after successful corneal implantation. Many tasks that were hard to do because of corneal disease become easier, which gives patients more independence and confidence.
Millions of people in the UK have corneal disease, but new transplantation techniques give real hope. Precision Vision London’s 92% vision improvement rate isn’t just a number – it represents life-changing results for patients who want better vision. Personalised treatment options are available if you face challenges with corneal disease. Precision Vision London combines surgical expertise, advanced technology, complete aftercare, and patient-focused approaches to give you the highest standard of care during your trip toward clearer vision.
Key Takeaways
Recent research demonstrates that corneal implants have achieved remarkable success rates, offering genuine hope for vision restoration to millions affected by corneal disease.
- New research shows 92% of patients achieve 20/200 or better vision following corneal implantation, representing a significant breakthrough in vision restoration technology.
- Different techniques suit specific conditions: PKP offers 92% long-term survival at 10 years, whilst DMEK provides faster recovery with 50% achieving 20/25 vision within 6 months.
- Surgeon experience dramatically impacts outcomes, with specialists performing over 300 procedures annually showing 40% fewer complications than less experienced practitioners.
- Advanced technologies like intraoperative OCT and femtosecond lasers improve precision, influencing surgical decisions in 40% of procedures and reducing complications significantly.
- Patient factors including age, pre-existing conditions, and fellow eye health substantially affect success rates, making comprehensive evaluation essential for optimal outcomes.
- Structured postoperative care with regular monitoring ensures long-term success, with most rejection episodes successfully reversed when detected early through proper follow-up protocols.
The combination of surgical expertise, advanced technology, and personalised treatment approaches has transformed corneal transplantation from a last resort into a highly successful vision restoration option, with patients reporting significant improvements in both visual acuity and quality of life.
FAQs
Q1. What is the success rate of corneal implants according to recent research? Recent studies show that 92% of patients achieve vision of 20/200 or better following corneal implantation. This represents a significant advancement in vision restoration technology and demonstrates the high success rates now possible with modern corneal transplant techniques.
Q2. How do different corneal transplant techniques compare in terms of outcomes? Different techniques suit specific conditions. Penetrating keratoplasty (PKP) offers 92% long-term survival at 10 years, while Descemet Membrane Endothelial Keratoplasty (DMEK) provides faster recovery with 50% of patients achieving 20/25 vision within 6 months. The choice depends on the specific corneal condition being treated.
Q3. What role does surgeon experience play in corneal implant success? Surgeon experience significantly impacts outcomes. Specialists performing over 300 procedures annually show 40% fewer complications than less experienced practitioners. This highlights the importance of choosing a highly experienced surgeon for corneal implant procedures.
Q4. How do advanced technologies improve corneal implant procedures? Advanced technologies like intraoperative Optical Coherence Tomography (OCT) and femtosecond lasers greatly improve surgical precision. These tools influence surgical decisions in 40% of procedures and significantly reduce complications, leading to better outcomes for patients.
Q5. What factors affect long-term success of corneal implants? Several factors influence long-term success, including the patient’s age, pre-existing conditions, and the health of the non-operated eye. Additionally, structured postoperative care with regular monitoring is crucial for ensuring long-term success and detecting any potential complications early.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

