Here’s a surprising fact – about 1 in 375 people in the UK live with keratoconus, an eye condition that can really affect their vision. Young adults, mostly in their late teens or early twenties, are the main group affected by this eye condition. Black and Asian populations show higher rates of occurrence. The good news is that early keratoconus cross-linking treatment in London can stop the condition from getting worse. Corneal cross-linking (CXL) stands out as the only proven medical procedure that stops keratoconus from progressing. The treatment works by making the natural ‘cross-links’ between collagen fibres in your cornea stronger.
The results speak for themselves – more than 90% of patients see their condition stabilise after one treatment. These numbers matter because before CXL became accessible to more people, up to 20% of keratoconus patients needed corneal transplants. Research shows that cross-linking works best when doctors catch and treat the condition before major changes happen to your cornea’s shape.
Precision Vision London focuses on early treatment with cutting-edge technology and personalised care. This piece will guide you through the cross-linking procedure from start to finish. You’ll learn why getting treatment at the right time is vital to protect your vision.

Understanding Early Keratoconus
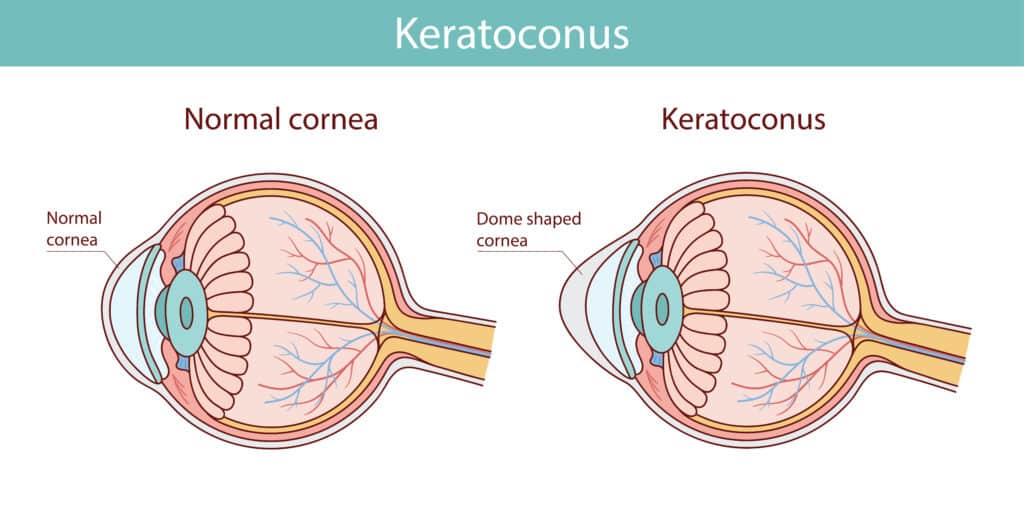
Keratoconus is a progressive eye condition where your cornea—the clear, front surface that protects your eye and helps you focus—becomes thin and bulges. Your normally round cornea changes into a cone shape and creates visual distortions that get worse over time.
What is keratoconus and how it progresses
Most people develop this condition in their teenage years or early adulthood. Doctors diagnose it most often between ages 20-30. The condition affects more people than we once thought up to 1 in 450 people in some populations. Your cornea starts thinning and changing shape in a distinctive pattern. These original changes might not affect your vision much. Your cornea steepens and bulges outward as the condition advances. This creates irregular astigmatism that glasses can’t fully correct. Changes happen faster earlier in life but usually stabilise around age 40-45. The biggest changes occur in the first 15-20 years after onset. The speed and severity vary among people, and your eyes often differ, with one eye usually worse than the other.
Why early detection is critical
Finding keratoconus early can save your vision. Detection before major corneal changes leads to better long-term results. Early diagnosis lets doctors use treatments like cross-linking to stop the condition from getting worse. Quick detection helps avoid serious complications. Poor early management can lead to severe corneal scarring, sudden corneal swelling (hydrops), and possible severe vision loss. Finding keratoconus before refractive surgery is vital since laser treatment on an undiagnosed keratoconic cornea could cause severe progressive iatrogenic ectasia. Precision Vision London uses sophisticated diagnostic technology to detect subtle corneal changes before they affect your vision. This allows earlier treatment and better visual outcomes.
Common signs and early topography changes
Early keratoconus symptoms might seem minor at first. You might notice:
- Vision getting worse in one or both eyes
- Blurry or distorted vision, especially in dim light
- More sensitivity to light and glare
- Your glasses prescription changing often
- Bright lights surrounded by halos
- Double vision in just one eye
Doctors can spot the first signs of early keratoconus through corneal topography. They look for the thinnest part of the cornea moving from its central position, a raised posterior corneal surface, and irregular corneal shape. Research shows the index of height decentration and index of vertical asymmetry work best to tell healthy eyes from early keratoconus. The D-index becomes more useful for diagnosing ectasia as the condition progresses. Corneal topography remains the best way to diagnose early keratoconus. It creates detailed maps of your corneal surface to find characteristic irregularities. These specialised scans can detect subtle changes before standard eye exams. Precision Vision London uses advanced corneal imaging to spot even the earliest signs of keratoconus. This lets us use cross-linking treatment when needed to protect your vision for years ahead.
Why Early Cross-Linking Matters
Corneal cross-linking has transformed how we manage keratoconus. This innovative procedure gives us a chance to treat the condition early. It helps preserve vision and prevents the need for more invasive treatments later.
Progression risk in the UK population
The prevalence of keratoconus in the UK shows why early cross-linking matters. Keratoconus affects 1 in 1,750 people across the UK. It occurs equally in males and females across all ethnic groups. In spite of that, some groups face higher risks. The prevalence rises to about 1 in 450 in people with South Asian backgrounds. Each person’s condition progresses differently. Keratoconus gets worse faster in your twenties and early thirties without proper treatment. Young patients with steeper corneal curvature face the highest risk of substantial progression. Our team at Precision Vision London recognises these risk factors. We monitor patients closely with full corneal topography examinations every few months, especially for younger patients.
Benefits of early intervention
Early-stage cross-linking treatment provides clear advantages. The procedure works better when performed during early keratoconus rather than advanced stages. The results speak for themselves clinical trials show cross-linking stops progression in more than 90% of treated eyes. Cross-linking can improve your corneal shape. It reduces corneal steepening and enhances visual acuity in many cases. Our team at Precision Vision London focuses on early detection and quick treatment. Our experience matches UK statistics that show treatment success rates of 95-98% with up to six years of follow-up care.

Avoiding corneal transplant through timely treatment
Before cross-linking existed, about 20% of keratoconus patients needed a corneal transplant. Timely cross-linking treatment has reduced this need substantially. Several countries report lower rates of keratoplasty for keratoconus since starting corneal cross-linking programmes. A corneal transplant works but requires long healing time. It needs ongoing topical medications and carries risks of glaucoma, cataracts, or graft rejection. Early cross-linking at Precision Vision London offers a safer approach with minimal complications. Your personal situation might allow combining cross-linking with other vision correction procedures after stabilisation. Early cross-linking keeps more treatment options open for your future visual needs. Our specialists at Precision Vision London assess your corneal topography to find the right time to treat. This ensures you get care before major corneal changes occur.
Step-by-Step: The Cross-Linking Procedure
Precision Vision London performs corneal cross-linking as an outpatient procedure. You can go home the same day. This simple treatment will give a stronger cornea and stops keratoconus from getting worse.
Preparing for your appointment
Your cross-linking procedure will work better with proper preparation. We recommend you:
- Eat and drink normally before your appointment
- Wear comfortable, loose-fitting clothing
- Arrange for someone to drive you home afterwards
- Remove contact lenses at least one day before surgery
- Plan to take 1-2 weeks off work for recovery
You should stay in the UK at least two weeks after treatment. This helps us provide follow-up care if needed.
What happens during the procedure
Your cross-linking procedure at Precision Vision London follows these steps:
- Your eye becomes numb with anaesthetic drops to keep you comfortable. The ophthalmologist then removes the thin outer layer of your cornea (epithelium) so the medication can penetrate better.
- Your cornea receives vitamin B2 (riboflavin) eye drops every 3 minutes for about 30 minutes. Once the saturation reaches the right level, your surgeon directs ultraviolet-A (UV-A) light at your cornea for around 30 minutes. During this time, you continue getting riboflavin drops.
- A protective bandage contact lens covers your eye until your first follow-up appointment, usually within 3-7 days.
How riboflavin and UV light work together
The photochemical reaction between riboflavin and UV light makes cross-linking work. Riboflavin has two jobs: it triggers new chemical bonds (cross-links) between collagen fibres in your cornea and absorbs 90% of UV-A radiation to protect deeper eye structures. These new cross-links substantially strengthen your cornea’s biomechanical properties and stop keratoconus from progressing. The riboflavin used in your procedure contains nowhere near the amount found in a single over-the-counter vitamin B2 supplement.
Types of cross-linking: standard vs accelerated
We offer both standard and accelerated cross-linking protocols at Precision Vision London:
- The standard protocol (Dresden protocol) uses UV-A exposure at 3 mW/cm² intensity for 30 minutes. This delivers a total energy of 5.4 J/cm². This 20-year-old method has the longest clinical track record.
- The accelerated cross-linking uses higher UV-A intensity (9 mW/cm²) for 10 minutes. It delivers the same total energy. Treatment time reduces while maintaining effectiveness.
- Both methods are a soaring win in stabilising keratoconus. Some studies suggest the standard protocol might work better for keratometry and astigmatism parameters.
Recovery and Aftercare at Precision Vision London
Your keratoconus treatment’s recovery phase is a vital part of the healing process. Precision Vision London will give a complete aftercare support throughout this process to ensure optimal healing and visual outcomes.
What to expect in the first 72 hours
The first 72 hours after the procedure can be challenging. Your eye will feel sore, gritty, and watery as with having something stuck in it. Your vision stays blurry during this time, which is normal while your cornea heals. Pain reaches its peak in the first 24-48 hours, and day 1 feels most intense. The discomfort should decrease by day 3. Your vision might get worse temporarily during these first days before it starts improving. A protective bandage contact lens stays in place for about a week to protect your healing cornea. This lens helps with comfort and proper epithelial regeneration.
Managing discomfort and light sensitivity
Light sensitivity (photophobia) happens often after cross-linking and can be intense at first. Here’s how you can manage it:
- Take rest in a darkened room with your eyes closed when possible
- Put on sunglasses, even indoors, to protect your eyes
- Take prescribed pain medication according to instructions
- Place cool compresses on closed eyes to reduce swelling
Keeping eye drops in the refrigerator can help soothe your eyes. You should use these drops every hour during the first day to keep your cornea lubricated properly.
Follow-up care and healing timeline
Your first check-up happens 3-7 days after treatment. Your specialist at Precision Vision London will check your healing progress and remove the bandage contact lens. Pain should go away completely by days 5-7 as your corneal epithelium grows back. Your vision gets better gradually over 2-3 weeks but might change for several months this is normal during healing. Regular check-ups continue at 1 month and 3 months after the procedure. These visits let our specialists track your corneal stability through detailed topography scans and help with any concerns.
When to resume contact lenses or glasses
Your vision stabilises enough to think over new glasses after 3-6 months. The timing for contact lenses depends on their type, Soft contact lens users should wait until they finish their steroid eye drops, usually 4 weeks after the procedure. People who use rigid gas permeable (RGP) lenses can start wearing them from the second week if healing goes well. Precision Vision London’s specialists will check your healing progress to decide when you can start wearing lenses again. We take a personalised approach that will give a smooth recovery with minimal disruption to your daily life.
Long-Term Results and Considerations
Corneal cross-linking provides amasing long-term stability for patients with early keratoconus. This treatment gives you peace of mind about your future vision.
Expected outcomes and success rates
Research shows that corneal cross-linking works really well. Success rates are over 90% in stopping keratoconus from getting worse. Our team at Precision Vision London matches these great results. About 94% of our patients’ corneas stabilise after just one treatment. Data collected over 10 years backs up these lasting results.
Potential risks and how we minimise them
Cross-linking is a safe procedure, but you should know about some possible risks:
- Temporary corneal haze that usually clears up within months
- Slower epithelial healing
- Infection happens rarely – about 1 in 1000 cases
- Vision loss affects less than 3% of patients
Our team at Precision Vision London uses careful sterilisation methods and personalised treatment settings to keep these already low risks to a minimum.
Ongoing monitoring and topography scans
Your treatment success requires regular check-ups for up to five years. These visits include vision tests, glasses prescriptions, and detailed corneal topography scans. The first scan happens at six months, then yearly after that. Regular monitoring helps us confirm your treatment keeps working.
When retreatment might be needed
Good news – very few patients need another treatment, less than 1%. All the same, younger patients might need retreatment because their corneas naturally regenerate over 7-8 years. The best part is that if your condition starts progressing again, you can safely get another cross-linking treatment.
Conclusion
Early keratoconus cross-linking is a breakthrough treatment that stops keratoconus from getting worse before your vision deteriorates. Without doubt, this procedure’s remarkable 90% success rate makes it the best way to protect your vision against this progressive condition. Your timing matters a lot in managing keratoconus. Advanced corneal topography helps detect it early, which substantially cuts down your chances of needing a corneal transplant later. Getting treatment as soon as you notice the first signs will give a better outcome and protect your vision.The cross-linking procedure is simple and minimally invasive. You might feel some discomfort and notice vision changes during recovery, but these usually clear up in a few weeks. The long-term benefits are worth these temporary issues, and most patients’ corneas stabilise after one treatment.
Precision Vision London’s team uses cutting-edge diagnostic technology with custom treatment plans to deliver great results. Our detailed aftercare programme helps you recover smoothly. We schedule regular check-ups to track how you’re doing. Our specialists focus on protecting your vision through quick action and expert care. Note that keratoconus affects 1 in 375 people in the UK, and some groups face higher risks. It’s vital to know your risk factors and get checked if you notice any vision changes. Starting cross-linking treatment early at Precision Vision London gives you the best shot at keeping your vision clear and stable for life.
Key Takeaways
Early keratoconus cross-linking offers a proven solution to halt vision deterioration, with over 90% success rates when performed promptly. Here are the essential insights for patients considering this treatment:
- Early detection is crucial – Cross-linking works best before significant corneal changes occur, preventing the need for corneal transplants in up to 20% of cases.
- The procedure is minimally invasive – Outpatient treatment using riboflavin drops and UV light takes about 90 minutes with same-day discharge.
- Recovery requires patience – Expect 2-3 weeks of blurred vision and light sensitivity, with full stabilisation occurring over 3-6 months.
- Long-term results are excellent – Over 90% of patients achieve corneal stabilisation after one treatment, with effects lasting 10+ years.
- Retreatment is rarely needed – Less than 1% of patients require additional cross-linking, making it a highly effective one-time intervention.
The key message is clear: if you’re experiencing vision changes or have been diagnosed with early keratoconus, prompt cross-linking treatment at a specialist centre like Precision Vision London can preserve your sight and prevent more invasive procedures later.
FAQs
Q1. How effective is early keratoconus cross-linking in preventing vision loss? Early cross-linking is highly effective, with success rates exceeding 90% in halting keratoconus progression. When performed promptly, it can significantly reduce the need for corneal transplants and preserve vision long-term.
Q2. What should I expect during the recovery period after cross-linking? The initial 72 hours post-procedure are typically the most challenging, with soreness, blurred vision, and light sensitivity. Most discomfort subsides within a week, but vision may fluctuate for several months as your eye heals.
Q3. How long does the cross-linking procedure take? The entire cross-linking procedure usually takes about 90 minutes. This includes the application of riboflavin drops for 30 minutes, followed by UV-A light exposure for another 30 minutes.
Q4. When can I resume wearing contact lenses after cross-linking? The timing varies depending on the type of lenses. Soft contact lens wearers typically wait about 4 weeks, while rigid gas permeable (RGP) lens users may begin reinsertion from the second week onwards, provided adequate healing has occurred.
Q5. How often will I need follow-up appointments after the procedure? Initial follow-ups occur within the first week, then at 1 month and 3 months post-procedure. Thereafter, regular monitoring continues for up to five years, with detailed corneal topography scans typically performed at six months and then annually.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

