Here’s a surprising fact – one out of every 375 people in the UK deals with eye rubbing keratoconus. Eye specialists in London take this condition very seriously because untreated cases can permanently damage your vision. Let’s talk about keratoconus. It’s a degenerative eye condition that thins your cornea and changes its shape to look like a cone. Research shows that chronic eye rubbing stands out as one of the most important risk factors. Your cornea becomes distorted at the time you keep rubbing your eyes, and this can end up causing permanent vision loss. The condition usually shows up in both eyes, but all eyes except one show more severe symptoms.
The good news? Early treatment can make all the difference. Doctors can stop keratoconus from getting worse with treatments like cornea collagen cross-linking. But dealing with the mechanisms of eye rubbing is a vital part of managing this condition for London patients. In this piece, you’ll find practical strategies that help you cut down on eye rubbing. These techniques will protect your vision and help you manage keratoconus better in your daily routine. You’ll learn to spot your personal triggers and find simple techniques that can make a big difference in your eye health.

Understanding Keratoconus and Eye Rubbing
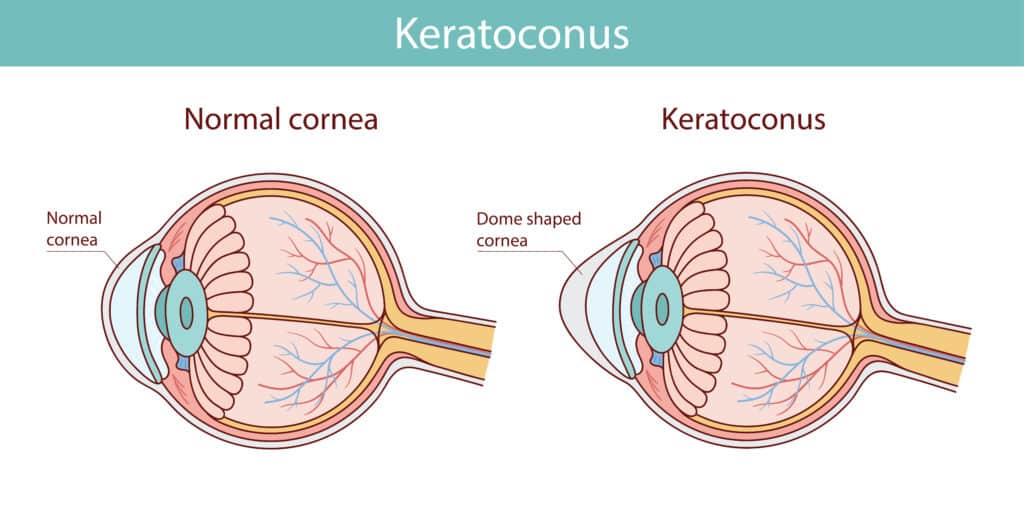
Keratoconus comes from Greek words “keras” (horn) and “konos” (cone), which perfectly describes this progressive eye disorder. Your normally dome-shaped cornea changes into an irregular cone-like protrusion that affects vision by a lot.
What is keratoconus and how it affects the cornea
Your eye’s clear front surface, the cornea, keeps a symmetrical dome shape to focus light onto the retina properly. A non-inflammatory process of corneal thinning and protrusion disrupts this balance. This condition affects all corneal layers. The corneal stroma (the thickest middle layer) shows the most notable changes. The thinning usually happens at the inferior or central portion of the cornea. This creates distortion and leads to the characteristic cone shape. The cornea’s refractive powers change dramatically, which causes visual impairment through induced myopia (short-sightedness) and irregular astigmatism. Research shows keratoconus affects both eyes in all but one of these cases, though severity and progression often develop unevenly. The prevalence ranges from 0.2 to 4,790 per 100,000 people worldwide. London eye specialists consider this a vital concern.
Why eye rubbing worsens keratoconus
Several years of research proves chronic eye rubbing makes keratoconus worse and can trigger its development. Here’s what studies reveal:
- 65.6% of keratoconus patients had a history of eye rubbing in one survey
- Eye rubbing showed up in 83% of keratoconus subjects compared to only 58% in healthy controls
- The way you rub matters – knuckle rubbing applies 9.6 N of force, which is 2.2 times more than fingertip rubbing (4.3 N)
Persistent eye rubbing creates mechanical trauma that triggers damaging processes. The cornea releases enzymes that weaken its shape-maintaining collagen fibres. Eye rubbing also raises corneal temperature and creates buckling and flexure of collagen fibrils. This helps form the cone and changes corneal biomechanical stability. Brief eye rubbing can reduce keratocyte density in human corneas. Research found that light eye rubbing for just 10 seconds, repeated 30 times over 30 minutes, reduced these vital corneal cells by a lot.
Common symptoms and early warning signs
You might not notice any symptoms when keratoconus first appears. However, these warning signs might show up:
- Vision gets worse and glasses don’t help much
- Bright objects appear with halos and light sensitivity increases
- Vision becomes blurry or cloudy over time
- Glasses prescription changes often
- One eye sees double images
- Dark environments make seeing harder
Eye care professionals can spot specific clinical signs as keratoconus develops:
- Fleischer’s ring: A brown-coloured iron deposit ring shows up at the cone’s base during examination
- Vogt striae: Vertical stress lines form when the Descemet membrane compresses in the cornea’s thinnest area
- Munson sign: Advanced cases show a V-shaped lower eyelid indentation during downward gaze from the protruding corneal cone
Keratoconus usually starts during puberty or early adulthood. It progresses until mid-30s and stabilises around age 40. Early detection and proper management help preserve vision. Regular detailed eye examinations at Precision Vision London can catch keratoconus early. This becomes especially important if you have risk factors like atopy (allergies, asthma, eczema) or family history.
Why Eye Rubbing Happens
Breaking the eye-rubbing cycle starts with understanding why your eyes itch. London patients experience several specific reasons that make them rub their eyes.
Allergy-related triggers in the UK
The UK’s climate creates perfect conditions that cause allergic reactions and eye rubbing. Your immune system overreacts to harmless substances in the environment, which results in allergic conjunctivitis. This reaction inflames the conjunctiva—the clear, thin membrane that covers the white of your eye.
Common triggers that cause eye rubbing include:
- Tree, grass, and weed pollens (hay fever is especially common in the UK)
- House dust mites
- Pet dander from cats and dogs
- Mould spores
- Air pollution in London’s urban environment
Your body releases histamines in the tissues around your eyes at the time allergens make contact. This causes itching, swelling, redness, and watering. Your body’s inflammatory response tries to eliminate irritants but creates an intense urge to rub. People who have keratoconus often deal with other allergic conditions like asthma and eczema. These conditions might make them more likely to rub their eyes.

Dry eyes and digital strain
Our modern lifestyle substantially increases the risk of dry eyes, which makes people rub their eyes more. Dry eye happens because of problems with tear production or quality, and this irritation makes people rub their eyes. Screen use has become a major reason for dry eye symptoms. A newer study, published by meta-analysis shows that between 9.5% and 87.5% of digital device users experience these symptoms. The problem got worse during COVID-19, with 64% of people in a French survey saying they used screens more during lockdowns.
Digital eye strain mainly happens because of changes in blinking patterns. Research shows people blink substantially less while using screens compared to when they’re resting. Less blinking means more tears evaporate, which creates a cycle of dryness and irritation that makes people rub their eyes. UK and Ireland residents show high rates of digital eye strain. The Computer Vision Syndrome Questionnaire reveals 62.6% of people experience symptoms, and they use devices for about 9.7 hours daily.
Stress and unconscious habits
People often rub their eyes to self-soothe when they feel anxious, stressed, or overwhelmed. This behaviour happens without thinking and often comes with other signs like fidgeting or avoiding eye contact. Fatigue and sleepiness can also make people rub their eyes without realising it. Eye specialists notice that people rub their eyes spontaneously at bedtime, when they wake up, or during times of eye fatigue or emotional stress. The number of keratoconus patients who rub their eyes ranges from 66% to 91%. Atopy and allergies remain the main risk factors that cause this chronic habit. Precision Vision London specialists use this knowledge to create personalised plans that help patients manage both keratoconus and why it happens.
Behaviour Change Strategies That Work
Breaking the eye-rubbing habit will give a structured path forward. You need to address your unique triggers and find practical alternatives. These evidence-based strategies can help protect your corneal health if you have keratoconus in London.
Identifying personal triggers
Your first step to changing this behaviour starts with understanding what makes you rub your eyes. A one-week “rubbing diary” Create yours here helps track these patterns. Note down when it happens, what you’re doing, and how you’re feeling at that moment. This awareness helps spot unconscious patterns. We noticed that allergens, digital eyestrain, or stress are common triggers. Many patients find they rub their eyes during specific activities or emotional states. This is a chance to target the root cause.
Using cold compresses and lubricating drops
Cold compresses quickly relieve itching without causing damage. Make an effective compress by soaking a clean cloth in cool water. Gently wring it out and place it on your closed eyelids for 10-15 minutes. A quick fix is wrapping frozen vegetables in a cloth. Remember not to put ice directly on your eyelids. High-quality lubricating drops are the life-blood of treatment. The best results come from preservative-free artificial tears like Refresh or Systane. Stay away from drops that claim to “get the red out” – they might make things worse. Your drops feel even better when kept in the refrigerator. The cool sensation helps relieve itching.
Replacing the habit with safer alternatives
Here are some non-damaging options to replace eye rubbing:
- Squeeze a stress ball or smooth stone when you feel the urge
- Take deep breaths during intense itching episodes
- Keep your hands busy with fidget toys at your desk
These distractions help train your brain to respond differently when your eyes itch.
Setting reminders and visual cues
Visual prompts can stop you from rubbing your eyes automatically. Small stickers on your computer or phone work great as reminders. The 20-20-20 rule helps too. Look at something 20 feet away every 20 minutes. Then take 20 seconds and do 20 careful blinks to rewet your eyes. This simple trick reduces digital eyestrain that often leads to rubbing.
Involving family or support systems
Your family members can help by letting you know when you’re rubbing your eyes. Most people don’t realise they’re doing it. This feedback catches what you might miss. Regular check-ups with specialists at Precision Vision London let them track your progress and fine-tune your approach. Their expertise in keratoconus management helps create a plan that works just for you.
Tools and Techniques to Reduce Eye Rubbing
Practical tools can make a big difference in managing keratoconus and reducing harmful eye rubbing. These techniques work alongside behaviour change strategies and give London patients real options to handle this challenging condition.
Cooling eye masks and stress balls
Cooling eye masks help relieve itchy eyes without causing damage from rubbing. The Optase Cooling Mask provides cooling therapy to closed eyelids and soothes symptoms like itchy, red, watery eyes caused by allergens such as hay fever, dust and animal hair. You should freeze these masks in a sealed bag for at least an hour, then apply them to closed eyes for about 10 minutes. The cooling sensation switches off your body’s inflammation response, which helps stop the itchiness. Stress balls are great alternatives that keep your hands busy. Squeezing a stress ball releases tension and gives you a healthy outlet instead of rubbing your eyes. Fidget toys like spinners or cubes can also keep your hands occupied and make you less likely to rub your eyes.
Allergy management tips for London patients
Refrigerator-cooled artificial tears help reduce allergy symptoms. The cold sensation brings relief while washing out allergens. Anti-histamines and mast-cell stabilisers in eye drops, used twice daily, help curb allergic conjunctivitis effectively.
Using preservative-free artificial tears
Preservative-free eye drops work well for keratoconus patients because they’re gentle on the eyes. Eye specialists often recommend products like Hylo-Tear that contains sodium hyaluronate. This creates a stable film on your eye surface for lasting relief. These drops give immediate comfort and stop the burning sensation that often makes people rub their eyes.
Practising the 20-20-20 screen rule
The 20-20-20 rule is a proven way to prevent digital eye strain. Look at something 20 feet away for 20 seconds every 20 minutes. This simple practise eases symptoms like dry eyes and visual discomfort, especially when you combine it with other healthy screen habits. Keratoconus patients who work long hours with digital devices find this rule helpful because it reduces eye fatigue that might lead to rubbing.
Monitoring Progress and When to Seek Help
Tracking your eye-rubbing habits plays a key role in keratoconus management. Technology has brought new ways to track your progress and tell you when it’s time to see a doctor.
How to track your eye rubbing habits
Modern AI-powered applications can now recognise, count and show how often you rub your eyes. These smart tools alert you through vibrations or sounds when they detect repeated rubbing. Simple self-assessment tools work well too. The Goodman score (≥5 in 63.2% of cases) and CAGE score (≥2 in 74.4% of patients) help you understand your eye-rubbing patterns. Regular tracking shows your patterns and lets you measure improvements.
When to consult a keratoconus specialist
You should see a specialist if:
- Your vision changes often even with glasses
- Light bothers you more than usual
- Your vision gets worse despite using anti-rubbing techniques
- You have conditions like eczema, asthma, or hay fever
Most cases don’t need urgent care since keratoconus progresses slowly.
What to expect during a clinic visit at Precision Vision London
Precision Vision London’s Harley Street clinic provides surgeon-led care throughout your treatment. Your appointment includes:
- Vision tests
- Refraction assessments
- Corneal scans
Dr Pillai, the clinic’s world-renowned corneal specialist, creates treatment plans that fit your specific needs. Every keratoconus treatment comes with a complete 12-month aftercare programme.
Conclusion
Keratoconus management needs a multi-pronged approach. Reducing eye rubbing is the life-blood of treatment that works. You can take control of your eye health by understanding how eye rubbing connects to corneal changes. Simple behaviour changes will bring substantial benefits to your corneal stability as time passes. Cool eye masks, preservative-free lubricating drops, and stress balls give you quick alternatives when you feel like rubbing. On top of that, tracking your habits reveals patterns that create chances to step in before lasting damage occurs. These small daily changes work alongside clinical treatments at Precision Vision London, where Dr Pillai and the team customise care throughout your treatment trip.
Note that successful keratoconus management combines expert medical care with your active role. The specialist team at Precision Vision London’s Harley Street clinic supports you with advanced corneal scanning, surgeon-led consultations, and detailed aftercare programmes. Breaking the eye-rubbing habit becomes both an achievable goal and a vital step to preserve your vision. Your eyes need professional guidance at the first sign of vision changes or ongoing discomfort. Quick action substantially improves outcomes for keratoconus patients. The condition brings challenges, but these behaviour change strategies paired with expert care from Precision Vision London’s specialists help maintain optimal corneal health and vision quality for years ahead.
Key Takeaways
Breaking the eye-rubbing habit is crucial for keratoconus patients, as chronic rubbing significantly worsens corneal damage and can lead to permanent vision loss.
- Eye rubbing affects 65-83% of keratoconus patients and applies damaging force that weakens corneal collagen fibres.
- Identify personal triggers through a weekly rubbing diary to track patterns related to allergies, digital strain, or stress.
- Replace rubbing with cooling eye masks, preservative-free artificial tears, and stress balls for immediate relief.
- Practise the 20-20-20 rule: every 20 minutes, look 20 feet away for 20 seconds to reduce digital eye strain.
- Seek specialist help at first signs of vision changes, light sensitivity, or frequent prescription changes
Early intervention and behaviour modification can halt keratoconus progression when combined with professional care. Simple daily changes like using cold compresses and involving family support systems create lasting protection for your corneal health.
FAQs
Q1. How can I effectively stop rubbing my eyes if I have keratoconus? Use preservative-free artificial tears for dryness, apply cold compresses, and keep stress balls or fidget toys handy to occupy your hands. Practise the 20-20-20 rule during screen time and involve family members to gently remind you when you’re rubbing unconsciously.
Q2. What activities should I avoid if I have keratoconus? Avoid excessive eye rubbing, wearing old or poorly fitting contact lenses, sleeping in contact lenses, and prolonged screen time without breaks. Also, manage eye dryness and allergies, and don’t skip regular eye check-ups with your specialist.
Q3. How can I track my eye-rubbing habits? Keep a weekly “rubbing diary” to note when and why you rub your eyes. Some AI-powered apps can detect and count eye-rubbing episodes. Self-assessment questionnaires like the Goodman score can also help evaluate your eye-rubbing behaviours.
Q4. When should I consult a keratoconus specialist? Seek professional help if you experience frequent vision changes despite wearing glasses, increased light sensitivity, or continued vision deterioration even after implementing anti-rubbing strategies. Also, consult if you have related conditions like eczema, asthma, or hay fever.
Q5. What can I expect during a clinic visit for keratoconus management? At a specialist clinic, you’ll undergo vision tests, refraction assessments, and corneal scans. The specialist will develop a personalised treatment plan based on your unique needs. Many clinics offer comprehensive aftercare programmes to support your ongoing management of keratoconus.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.

