Cataracts affect millions of people around the world, especially when they get older. Most people know about blurry vision and colour changes as symptoms, but many patients ask if cataracts can trigger headaches and other uncomfortable symptoms.
My experience as an eye care professional shows how patients often develop eye strain from cataracts that can lead to tension headaches. This happens most often after they spend time reading or working on computers. Research supports this connection too – a 2008 study in the Journal of Headache and Pain pointed to a possible link between cluster headaches and cataracts, though scientists need to study this further.
Let’s explore how cataracts and headaches are connected, their impact on your vision, and why getting the right diagnosis is vital to finding relief.
The Science Behind Cataracts and Headaches
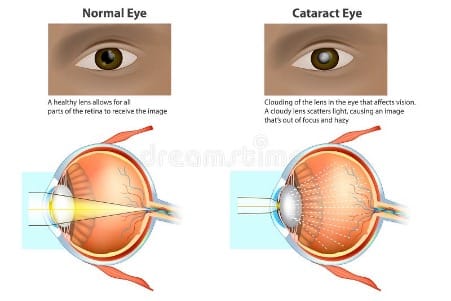
Image Source: Dreamstime.com
Many people think cataracts directly cause headaches, but that’s not actually true. The vision changes from cataracts can lead to head discomfort in several ways. Science shows that proteins in your eye’s lens break down and clump together, which creates cloudy areas that block and scatter light. Your retina can’t receive a clear image because of this. Your visual system has to work harder to make sense of the unclear information.
People with cloudy vision often try to compensate without realising it. Some people squint to see better, which creates tension in their forehead and eye muscles. Others lift their eyebrows to let more light reach their eyes. These actions can lead to headaches.
Cataracts change the way light bends through your eye’s lens. This makes your current glasses prescription less effective, and your eyes have to work overtime. A 2008 study in the Journal of Headache and Pain suggested a possible connection between cluster headaches and cataracts. Scientists need to research this connection more.
Light sensitivity becomes worse with cataracts. Bright environments become uncomfortable due to the cloudy lens, which can trigger or worsen headaches. This affects migraine-prone people even more. Cataracts affect depth perception too, which leads to eye fatigue during detailed tasks. Your eyes constantly adjust to worsening vision, which creates tension headaches.
The cloudy lens itself doesn’t cause pain. Your body’s response to seeing through it creates the perfect environment for headaches to develop. This makes the relationship indirect – it’s about how your visual system adapts to these challenges.
Why Your Cataracts Might Be Causing Head Pressure?
The relationship between cataracts and headaches runs deeper than just simple vision changes. Your visual system works overtime to compensate as the lens becomes progressively cloudy.
Eye Strain: The Main Culprit
Cataracts don’t directly cause headaches, but the visual strain they create definitely can. Your eyes struggle constantly to focus through the cloudy lens as vision deteriorates. This constant struggle triggers tension headaches because your eye muscles work too hard to achieve clarity.
Patients develop compensatory behaviours without realising it, which makes their headaches worse. You might catch yourself squinting or raising your eyebrows to see better. These unconscious habits create extra tension in your forehead and eye muscles that shows up as head pain.
Beyond Visual Strain
Your eyes become much more sensitive to light with cataracts, which often triggers headaches. This sensitivity becomes especially problematic around bright lights or when dealing with glare. On top of that, it affects your depth perception and tires your eyes during tasks that need precise vision. Cataracts can indirectly raise your eye’s internal pressure. The condition itself doesn’t directly increase eye pressure, but it can narrow your eye’s drainage angle and restrict fluid flow. Some people experience head discomfort from these pressure changes.
The connection goes beyond your eyes, and that’s fascinating. Research shows cataracts affect brain function – patients with poor vision from cataracts experienced decreased brain function and reduced grey matter volume. Your brain works harder to compensate for reduced visual input, which can trigger headaches.
The silver lining? Cataract surgery usually fixes these secondary symptoms. Your eyes can see clearly without straining after surgery, which removes a major headache trigger. Research confirms that cataract surgery reverses brain changes in both visual and cognitive areas linked to declining vision. This explanation helps us understand why many people feel relief from their chronic headaches after cataract treatment.
Diagnosing the True Source of Your Headaches
Professional evaluation becomes crucial to determine the true cause of headaches that occur with vision problems. Many patients think cataracts cause their head pain, but these symptoms usually have more complex origins.
Your doctor will start with a complete medical history and ask about how long symptoms have lasted, their severity, and the way lighting affects your vision. This discussion helps differentiate between cataract-related discomfort and other conditions that show similar signs.
Several specialised tests help diagnose cataracts. A visual acuity test shows how well you see objects from various distances. Your doctor might also conduct a slit-lamp examination using a microscope with an intense light beam to light up your eye’s front structures. This test usually reveals the characteristic clouding in your lens.
Headaches with visual symptoms could point to something completely different. Ocular migraines, retinal migraines, or even more serious conditions can look like cataract symptoms. Medical attention becomes urgent if you experience visual changes in just one eye, symptoms that last less than five minutes or more than an hour, or new headaches starting after age 50 .
The main concern arises from visual changes without headaches or the other way around. These symptoms might indicate:
- Retinal tears or detachments that can cause flashing lights and need immediate treatment
- Stroke that doctors sometimes confuse with migraine symptoms
- Glaucoma that doctors can check through tonometry tests measuring eye pressure
People who experience persistent headaches along with cataract symptoms usually develop them from eye strain rather than the cataract itself . Your eyes work harder as your vision becomes cloudier, which can trigger tension headaches.
Your doctor might dilate your pupils to get a full picture of your retina and optic nerve. This approach will give a precise diagnosis and help distinguish between simple eye strain from cataracts and serious conditions that need urgent care.
Note that new, severe headaches should prompt you to seek medical evaluation whatever your cataract status. Vision problems and head pain share complex connections that need professional assessment to identify their true source.
Conclusion
Cataracts and headaches often occur together, and their connection helps explain why patients experience both conditions simultaneously. Cataracts don’t cause headaches directly, but their effect on vision creates a chain reaction that leads to eye strain and head pain.
Research shows that proper cataract treatment can eliminate these related symptoms. Patients experience relief from headaches after cataract surgery because their eyes no longer deal with cloudy vision. The benefits go beyond improved sight – better brain function and reduced cognitive strain follow.
Accurate diagnosis and early treatment make all the difference. Headaches can indicate many conditions, but professional evaluation determines whether cataracts contribute to your symptoms. If cataracts affect your vision or that of your loved ones, Precision Vision London in Harley Street offers exceptional cataract treatment.
Note that you should never ignore headaches that occur with vision changes. Early intervention and expert care lead to better outcomes and protect your eye health long-term.
FAQs
Q1. Can cataracts directly cause headaches?
While cataracts don’t directly cause headaches, they can lead to eye strain and vision changes that may trigger headaches. The cloudy lens forces your eyes to work harder, potentially resulting in tension headaches, especially after visually demanding activities.
Q2. What are the early signs of cataracts?
Early signs of cataracts include cloudy or blurry vision, increased sensitivity to light, difficulty seeing at night, and faded or less vibrant colours. You may also notice glare or halos around lights and find it harder to read or perform detailed tasks.
Q3. How do cataracts affect daily activities?
Cataracts can significantly impact daily life by making it harder to see clearly, especially in low light conditions. They can affect depth perception, increase light sensitivity, and make it challenging to perform tasks that require precise vision, such as reading or driving.
Q4. Can cataract surgery alleviate headaches?
Many people experience relief from chronic headaches after cataract surgery. By restoring clear vision, the surgery eliminates the need for your eyes to strain, potentially reducing a key trigger for headaches associated with cataracts.
Q5. When should I see a doctor about cataracts and headaches?
You should consult an eye care professional if you experience persistent vision changes, increased light sensitivity, or frequent headaches, especially after visual tasks. New or severe headaches, particularly if accompanied by sudden vision changes, warrant immediate medical attention to rule out more serious conditions.
References
- https://pubmed.ncbi.nlm.nih.gov/23486235/
- https://www.healthinaging.org/a-z-topic/cataracts/tests
- https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
- https://www.aao.org/eye-health/ask-ophthalmologist-q/can-cataracts-cause-headaches
- https://www.webmd.com/eye-health/photophobia-facts
- https://www.sciencedirect.com/science/article/pii/S2352396418300860
- https://altoida.com/blog/is-there-a-connection-between-cataracts-and-dementia/
- https://www.mayoclinic.org/diseases-conditions/migraine-headache/expert-answers/ocular-migraine/faq-20058113
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

