The UK performs over 325,000 cataract surgeries each year. Preoperative tests are a vital step in your treatment plan. These complete assessments determine your candidacy and shape your surgical plan. Your pre-operative appointment involves several tests by an Ophthalmic Consultant to review your eye health and check cataract development.
A detailed pre op assessment comes before surgery scheduling. The examination lets specialists understand the severity of your cataracts and determine the best treatment approach for optimal results. Your pupils will be dilated with painless eye drops that might blur your vision temporarily. You should arrange for someone else to drive you to and from the appointment. These detailed evaluations have led to soaring success rates. More than 90% of patients see major improvements in their vision. On top of that, these tests help reduce risks. The chance of bleeding at the back of your eye during surgery is nowhere near common – just 1 in 10,000 cases.
This piece will help you find all the key preoperative tests for cataract surgery. You’ll learn what happens during each examination and how these tests support the roughly 10 million successful cataract surgeries worldwide every year.

Pre-Assessment Preparation for Cataract Surgery
Your pre-assessment appointment results will be accurate when you prepare the right way. The tests will determine if your cataracts are bad enough for surgery. The way you prepare affects how precise your preoperative tests turn out.
Bringing your current glasses and prescriptions
You need to bring both your distance and reading glasses to your pre-assessment appointment. Your eye specialist needs to check your current spectacles’ strength during evaluation. A copy of your recent prescription will also help if you have one. These measurements give baseline information that helps calculate your artificial lens implant’s strength (intraocular lens or IOL).
Contact lens removal timeline before testing
Contact lenses change your cornea’s shape temporarily and this can substantially affect measurement accuracy. So you must stop wearing contact lenses before your pre-assessment appointment:
- Soft contact lenses: Remove 48 hours to 2 weeks before your appointment (most NHS trusts recommend 2 weeks)
- Hard contact lenses: Remove 2-4 weeks before your appointment
Wrong corneal measurements can happen if you don’t follow these guidelines. This could lead to incorrect IOL power calculations and disappointing vision after surgery. Precise measurements determine the right artificial lens, making this step crucial.
Medication and medical history disclosure
Your medical history and current medications play a vital role during the pre-assessment phase. You should:
- Bring a complete list of your current medications
- List all tablets, eye drops, inhalers and supplements
- Tell us about any allergies
- Let specialists know about blood-thinning medications
- Bring your INR record book if you take warfarin
- Have your record book ready if you’re diabetic
Some medications might need adjustment before surgery, especially when you have medications that increase bleeding risk. But never stop taking prescribed medication without asking your doctor first.
Your complete medical history matters, including chronic conditions like asthma, back pain, or prostate problems. This information helps create a cataract surgery plan that fits your health needs.
Essential Eye Tests Before Cataract Surgery
A full picture of your eye health serves as the life-blood of preoperative tests needed for cataract surgery. These tests help specialists determine the severity of your cataracts and create a personalised surgical plan.

Visual acuity and refraction testing
Your vision test starts with a Snellen chart—the familiar letter chart eye doctors use. Reading letters from the top line down helps measure both your uncorrected vision and best-corrected visual acuity (BCVA) with glasses. These baseline measurements help determine if your vision qualifies you for surgery. Standards differ among practises. Most NHS trusts look at vision worse than 20/40 to 20/50 as a requirement for cataract surgery, along with noticeable decrease in vision.
Your pre-op assessment includes a vision test that shows your exact prescription. This documents how much your vision improves with correction. Medicare and most insurance providers need BCVA documentation before they approve surgery. Your doctor might also test how light affects your vision—a common issue with cataracts.
Intraocular pressure measurement to rule out glaucoma
The specialists will check the pressure inside your eyes to assess eye health and screen for glaucoma. This painless procedure uses anaesthetic drops in each eye. A handheld tonometer lightly touches the surface to give a digital pressure reading. This test becomes crucial if you have a history of high eye pressure or glaucoma, as pressure needs to be under control before surgery.
Slit-lamp examination for cataract type and severity
A slit-lamp examination gives doctors a detailed look at your cataract’s type and severity. Your ophthalmologist uses this specialised microscope to review your lens and grade the cataract using standardised systems like the Lens Opacities Classification System III (LOCS III). This classification reveals the extent of lens opacity and helps plan the surgery.
Doctors also check your pupil’s response, anterior chamber depth, and endothelial cell count during this examination. These critical factors influence the surgical approach. They look for small pupils that might complicate surgery and assess your cornea’s health. Lower endothelial cells increase the risk of corneal decompensation.
Biometric and Imaging Tests for IOL Planning
Precise measurements to select intraocular lens (IOL) are vital preoperative tests needed for cataract surgery. These detailed assessments help ensure your replacement lens gives you the best possible vision after surgery.
Axial length and keratometry in biometry
The right IOL power depends on accurate biometry measurements. The axial length (AL), which measures the distance between your cornea and retina, determines most of your refractive error. Every 1mm change equals about 3.00D of vision change. Your lens power needs depend on this measurement and keratometry (K) readings that show your corneal curvature.
Modern surgeons prefer optical biometers over ultrasound methods. The IOLMaster and similar devices use partial coherence interferometry with infrared laser light to give accurate, consistent measurements. AL and K values share an interesting relationship. Eyes with longer axial lengths usually have flatter corneas, while shorter eyes tend to have steeper corneal curves. Each unit increase in axial length leads to a 0.548 decrease in mean K.
Corneal topography for astigmatism detection
Detailed maps of your cornea’s surface come from corneal topography, which helps identify astigmatism patterns. This test shows the difference between regular astigmatism (symmetric bow-tie pattern) and irregular astigmatism (asymmetric or skewed patterns). This matters because about 40% of patients have irregular astigmatism, which affects whether toric IOLs will work.
The topographic assessment spots subtle corneal problems like early keratoconus, epithelial basement membrane dystrophy, or signs of previous refractive surgery that standard exams might miss.
OCT scan for macular health assessment
Optical Coherence Tomography (OCT) screening finds macular problems that could limit vision after surgery. OCT shows hidden macular pathology in about 13.7% of eyes that look normal in standard fundoscopic exams. This means doctors find one additional problem for every 7.3 eyes they screen.
OCT works especially well to find epiretinal membranes, vitreomacular traction, and age-related macular degeneration. These conditions often go unnoticed yet can substantially affect surgical outcomes. The findings change the surgical plan completely in about 0.83% of cases.
Systemic Health Checks for Surgical Safety
Cataract surgery requires more than just eye examinations. Several preoperative tests check your overall health to ensure a safe procedure. The surgery carries low risks, but specific health checks help identify possible complications.
Blood pressure thresholds before surgery
Your blood pressure readings are vital for surgical safety. Most eye doctors delay surgery if your diastolic blood pressure goes above 100 mmHg or your systolic pressure rises above 160-180 mmHg. Medical professionals call readings that stay above 160/100 mmHg poorly controlled.
Surgery gets postponed until your blood pressure stabilises if systolic readings exceed 180 mmHg or diastolic tops 110 mmHg. This careful approach exists because high blood pressure increases risks during surgery, such as hypertensive crises and retrobulbar haemorrhage.
A single high reading doesn’t mean automatic cancellation. Many patients show “white coat hypertension” during medical visits. Your surgical team might ask for home readings or 24-hour monitoring results in these cases.
Blood sugar levels in diabetic patients
Diabetic patients need proper blood glucose management before cataract surgery. Most surgeons want fasting blood sugar levels below 140 mg/dL and postprandial levels under 200 mg/dL, though no universal cut-off exists. Good diabetes control matters because high blood sugar affects wound healing and raises infection risks. You should take your regular diabetic medications before surgery unless your doctor says otherwise.
Modern practise no longer requires HbA1c measurement before cataract surgery. The Royal College of Ophthalmologists believes diabetic patients should control their blood sugar, but lacks evidence to cancel surgery above specific blood sugar or HbA1c levels.
When ECG or blood tests are required
Modern cataract surgery doesn’t need routine preoperative blood tests and ECGs. A complete Cochrane Review of 21,531 cataract surgeries found no fewer medical problems with routine preoperative testing.
Blood tests become necessary in specific cases. You’ll need an ECG if you have heart disease, blood glucose testing for diabetes, and potassium tests if you take diuretics. Blood-thinning medication users need an INR blood test the week before surgery. This focused testing approach reduces costs while keeping safety standards high.
Conclusion
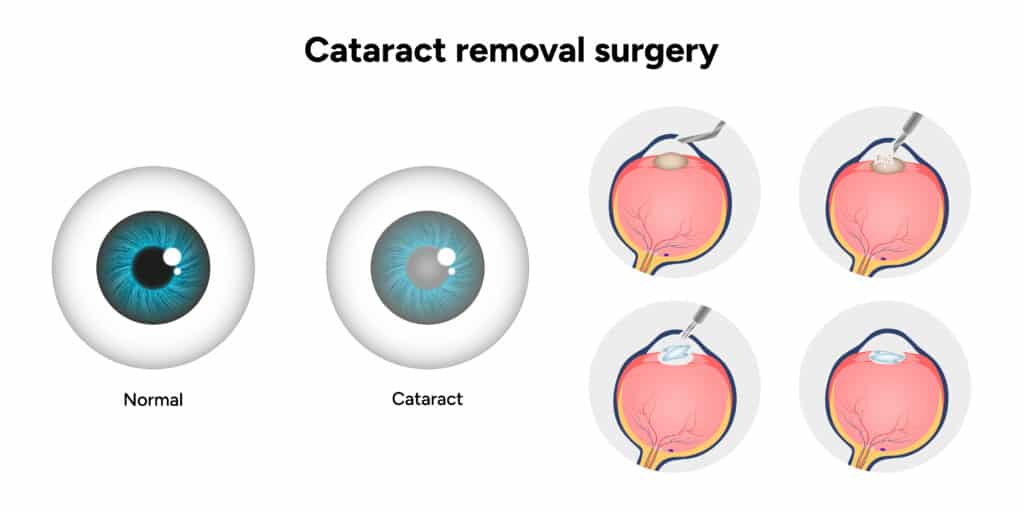
Complete preoperative tests are the foundations of successful cataract surgery outcomes. This piece explores everything you need to know about tests that determine your eligibility and help create a personalised surgical plan. Your eye health measurement, lens opacity assessment, and replacement lens power calculations work together seamlessly.
The preoperative process wants to maximise safety and effectiveness while reducing complications. Your surgeon can select the best intraocular lens by carefully measuring axial length, corneal curvature, and detecting any macular problems. Health evaluations also help identify factors that might affect your surgical experience.
You can take the next step toward clearer vision today. Schedule your complete cataract assessment with Precision Vision London to prepare fully for a successful surgery.
Our detailed preoperative testing approach explains cataract surgery’s impressive success rates. Each examination provides crucial information that contributes to the remarkable 90% patient satisfaction rate. Your active participation in the preoperative process shapes your visual outcome and becomes a great investment in your future eye health.
FAQs
Q1. How long before cataract surgery should I stop wearing contact lenses? For soft contact lenses, remove them 2 weeks before your pre-assessment appointment. If you wear hard contact lenses, you should stop wearing them 2-4 weeks prior. This ensures accurate corneal measurements for your surgery.
Q2. What vision tests are performed before cataract surgery? Pre-operative tests include visual acuity assessment using a Snellen chart, refraction testing to measure your exact prescription, and glare testing. These help determine the severity of your cataracts and guide treatment planning.
Q3. How is the correct intraocular lens (IOL) power determined? The IOL power is calculated using biometry measurements, including axial length and keratometry readings. Advanced optical biometers provide precise measurements of your eye’s dimensions to select the most suitable lens power.
Q4. Are blood tests necessary before cataract surgery? Routine blood tests are not typically required for cataract surgery. However, specific tests may be needed in certain circumstances, such as blood glucose testing for diabetic patients or INR tests for those on blood-thinning medications.
Q5. What blood pressure levels are considered safe for cataract surgery? Generally, surgery may be delayed if your blood pressure consistently exceeds 160/100 mmHg. Readings above 180/110 mmHg usually result in postponement until better blood pressure control is achieved. However, a single high reading due to anxiety doesn’t necessarily mean cancellation.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.
