Keratoconus affects 1 in 200 people globally and remains the leading cause of sight loss in young adults. London specialists provide Advanced Keratoconus Treatment options that offer hope to people struggling with this progressive eye condition. Most patients receive their diagnosis in their late teens or early twenties, and without treatment, keratoconus can substantially affect their vision quality and daily life.
Treatment options for keratoconus patients in the UK have evolved substantially. cross-linking (CXL) has proven effective for over 90% of patients by stopping the condition’s progression. Research shows the long-term stabilisation success rate of cornea collagen crosslinking ranges between 85-95%. Children with more aggressive keratoconus show vision improvement and stabilisation in about 82% of treated eyes.
Precision Vision London manages your keratoconus experience with state-of-the-art equipment and expert care. Our team uses advanced diagnostic tools and creates personalised treatment plans. This complete care will give you the most suitable intervention for your specific condition. This piece outlines treatment options, eligibility requirements, and expected outcomes during your treatment experience with our specialist team.

Understanding Advanced Keratoconus and Its Progression
Advanced keratoconus marks a critical phase where the cornea undergoes pronounced structural changes and vision gets worse. Medical professionals need to recognise this stage to determine if patients need aggressive treatment.
What defines advanced keratoconus?
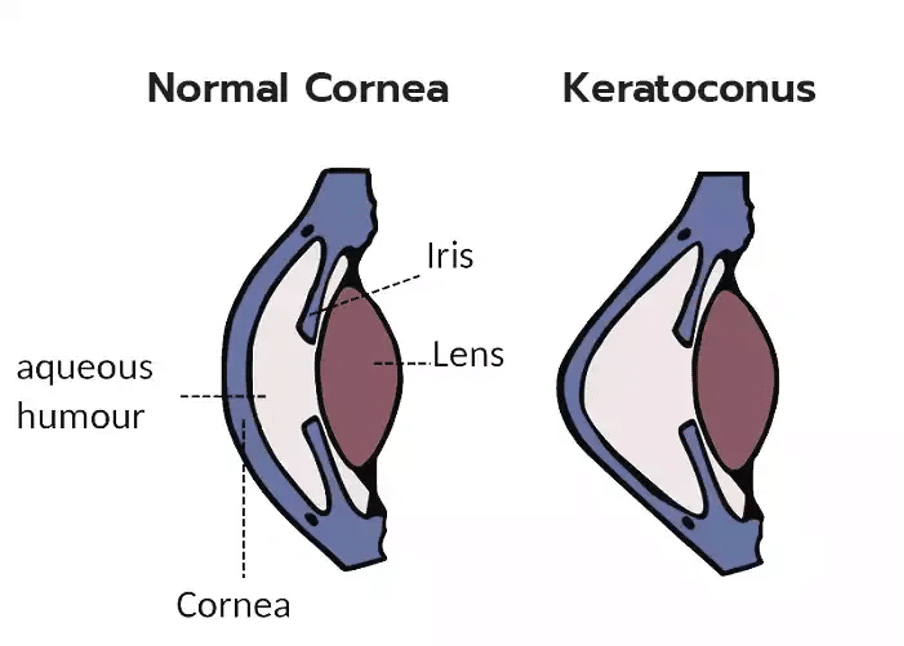
The cornea shows substantial distortion with moderate to major changes in advanced keratoconus. Your normally round cornea thins out and bulges outward into a cone shape. These structural changes lead to irregular astigmatism that affects your vision quality.
The hallmarks of advanced keratoconus include:
- Substantial corneal thinning and steepening
- Pronounced bulging of the corneal tissue
- Slight to moderate corneal scarring
- Dramatic deterioration in vision quality
Advanced cases show visible signs of corneal scarring, especially where the cone protrudes most. Many patients find it hard to achieve good vision even with standard glasses or regular contact lenses.
Common symptoms and diagnostic indicators
Symptoms become more noticeable and disrupt daily life as keratoconus advances. Patients often experience. Blurred or distorted vision affects routine activities severely. People struggle to recognise faces. They see multiple images (ghosting) and become extremely sensitive to light. Bright lights create halos that make night driving especially difficult.
Doctors use several sophisticated techniques to diagnose advanced keratoconus. Corneal topography maps out the cornea’s surface in detail and reveals irregularities typical of keratoconus. Pachymetry shows how thin the cornea has become. Specialists use slit lamp examination to check for corneal scarring, Fleischer rings (iron deposits forming rings within the cornea), and Vogt striae (stress lines from corneal stretching).
Why early intervention matters in keratoconus UK cases
Detecting and treating keratoconus early remains vital even in advanced stages. The condition usually starts in teenagers or young adults in their twenties and progresses slowly over 10 years or more. The risk of permanent vision loss goes up without treatment. UK statistics show keratoconus affects more people than we thought – about 1 in 450 people. Regular eye exams help catch it early.
Early intervention provides multiple benefits:
- Stops the cornea from getting worse
- Helps maintain better vision
- Reduces the need for corneal transplants
- Keeps corneal tissue healthy
Modern diagnostic technology helps specialists spot corneal changes before they affect vision. This allows them to start stabilising treatments right away.
Eligibility and Pre-Treatment Evaluation at Precision Vision London
Successful keratoconus management at Precision Vision London depends on detailed evaluation. The specialists review your eligibility and create a personalised treatment plan that lines up with your specific condition before suggesting advanced keratoconus treatment.
Corneal topography and tomography for diagnosis
Diagnostic precision at Precision Vision London relies on both corneal topography and tomography. Topography maps the anterior corneal surface to identify irregularities and astigmatism. The corneal tomography provides a three-dimensional analysis of the entire cornea, which includes thickness mapping and posterior surface review. This difference is significant because early posterior corneal changes often appear before visible anterior surface abnormalities.
The clinic uses multiple diagnostic technologies:
- Scheimpflug imaging creates detailed three-dimensional representations of corneal structure
- Anterior segment OCT provides high-resolution analysis of corneal epithelial thickness patterns
- Computerised corneal mapping produces qualitative and quantitative characterisation of corneal morphology

Minimum corneal thickness and other safety thresholds
Corneal thickness is a vital safety parameter for keratoconus treatments. Conventional corneal cross-linking (CXL) needs a minimum corneal thickness of 400 microns after epithelium removal to prevent endothelial toxicity. About 25% of keratoconus patients have corneas thinner than this threshold. Precision Vision London offers modified protocols for patients with thin corneas. Research shows successful outcomes that stop progression even in corneas as thin as 214 microns with specialised techniques.
Assessing progression through refraction and imaging
Treatment decisions depend on identifying progression. Precision Vision London reviews multiple parameters:
Objective markers of progression include:
- Increase of 1D or more in steepest keratometry over 1 year
- Increase of 1D or more in manifest cylinder
- Increase of 0.5D or more in spherical equivalent
- Progressive thinning of corneal thickness
The clinic follows global consensus guidelines that define progression as consistent change in at least two parameters: steepening of anterior corneal surface, steepening of posterior corneal surface, or progressive corneal thinning. Advanced imaging technologies help detect changes early. This detection becomes particularly important since about 25-30% of keratoconus cases show progression.
Advanced Keratoconus Treatment Options Available in London
London provides advanced solutions for patients with advanced keratoconus who want to restore their vision and stabilise their corneas. Each treatment option targets specific parts of the condition based on how severe it is and what each patient needs.
Epithelium-Off Corneal Cross-Linking (CXL)
This main treatment stops keratoconus from getting worse with a success rate exceeding 90%. The procedure makes corneal collagen fibres stronger by using ultraviolet light and riboflavin drops to stabilise the cornea. Accelerated CXL delivers the same UV light energy in just eight minutes instead of the standard 30 minutes, which might be safer for patients.
Topography-Guided Laser Treatment with CXL
This combined treatment stabilises the cornea and reshapes it to improve vision. Research shows big improvements in uncorrected and best-corrected visual acuity with more than two-line improvement in 23/30 and 17/30 cases respectively. The procedure removes tissue carefully to flatten steep areas and steepen flat areas.
Intracorneal Ring Segments (ICRS) for corneal reshaping
ICRS implantation puts small arc-shaped implants into the cornea to flatten and regularise its shape. About two-thirds of patients see better vision after treatment. Doctors have performed this minimally invasive procedure on more than 500,000 eyes worldwide.
Implantable Collamer Lens (ICL) for refractive correction
ICLs work great for stable, non-progressive keratoconus. Clinical studies show amazing results – the median uncorrected distance visual acuity improves to 20/25, and 40.6% of patients can see 20/20. These lenses sit between the iris and natural lens, making it possible to reverse the correction of refractive errors.
KeraNatural biologic inlays for structural support
KeraNatural uses donor corneal tissue that naturally merges with your eye’s structure, unlike synthetic implants. Studies show most patients improve their visual acuity by 3-4 lines, and about 60% get at least two lines better. This innovative approach reshapes the cornea to a more regular, stable curve without using synthetic materials.
Corneal Transplant for end-stage keratoconus
Doctors save corneal transplantation for cases where other treatments can’t correct vision. The procedure replaces the misshapen central cornea with donor tissue. Nearly 80% of patients can see well enough to drive within a year after surgery. The results are excellent – 95% of transplants stay clear for at least five years.
What to Expect During and After Treatment
Advanced keratoconus treatment might seem overwhelming at first. Understanding each step of the trip will help ease your concerns. Precision Vision London will give a comfortable experience throughout the whole process.
Step-by-step overview of the CXL procedure
The corneal cross-linking procedure usually takes 30-60 minutes as an outpatient treatment. Your eye gets anaesthetic drops to keep you comfortable. The doctor removes the epithelium (outer layer of the cornea) gently, often using a specialised instrument or laser (PTK) to improve outcomes. Riboflavin (vitamin B2) drops go into your eye every few minutes for 10-20 minutes. This allows the corneal tissue to absorb it. A controlled ultraviolet light targets your cornea for about 8-10 minutes to activate the riboflavin. A protective “bandage” contact lens covers your eye at the end.
Post-operative care and healing timeline
Right after the procedure, you’ll get antibiotic drops, anti-inflammatory drops, and lubricating drops among other pain medication. The bandage contact lens stays on for about 5-7 days until your epithelium grows back. You must follow a strict eye drop schedule. Drops go in every hour on day one, then less often as healing continues. Most people recover fully in several weeks, though complete stability takes 3-6 months.
Vision recovery expectations and follow-up schedule
Your vision will be blurry right after treatment and might change for several months. You’ll notice gradual improvements after 3-4 days, with most important changes within 7-14 days. In spite of that, vision usually stabilises in 2-3 months. You might need new glasses or contacts then. Your doctor will see you one week after treatment, then monthly for several months, with detailed check-ups at three months.
Managing discomfort and light sensitivity
The first 48 hours after the procedure challenge patients the most. Pain relief works better with prescribed pain relievers, cool compresses on closed eyes, cold eye drops, and rest in dark rooms. Sunglasses help with light sensitivity both indoors and outdoors. Call your doctor right away if pain increases 3-4 days after the procedure. This might indicate infection, though such complications rarely occur, affecting less than 1% of patients.
Conclusion
Precision Vision London provides proven solutions and hope for patients who don’t deal very well with progressive eye conditions like keratoconus. This piece explores various treatment options available at the centre. Each option targets different stages of keratoconus. Getting from diagnosis to treatment can feel overwhelming. The good news is that corneal cross-linking has success rates exceeding 90%. Treatments like topography-guided laser combined with CXL showed remarkable improvements in patients’ visual acuity.
Keratoconus affects about 1 in 450 people across the UK. Each case needs personalised care because symptoms vary among patients. Precision Vision London’s specialists recognise this reality. They use innovative technology like Scheimpflug imaging and anterior segment OCT to create treatment plans that match your eye’s specific needs.
Precision Vision London’s expert team stays committed to your comfort and best possible outcomes. You’ll get detailed support through every step – from pre-treatment evaluation to post-operative care. Early intervention is vital when you notice vision changes or receive a keratoconus diagnosis. Quick action reduces your chances of needing invasive procedures and helps maintain better vision quality over time.
Living with keratoconus brings challenges. But modern treatments have changed outcomes for patients dramatically. Precision Vision London’s specialists blend clinical excellence with compassionate care. This gives patients access to the UK’s most advanced treatments. Your vision matters. Choosing a specialist centre with proven expertise in managing keratoconus is essential. Precision Vision London stands at the vanguard of keratoconus care. The centre offers practical solutions and hope to patients at every stage of this condition.
FAQs
Q1. What is keratoconus and how common is it in the UK? Keratoconus is an eye condition where the cornea thins and bulges into a cone shape, affecting vision. It affects approximately 1 in 450 people in the UK, making it more common than previously thought.
Q2. What are the main symptoms of advanced keratoconus? Advanced keratoconus typically causes severely blurred or distorted vision, increased light sensitivity, difficulty with night driving due to halos around lights, and challenges in everyday activities like recognising faces.
Q3. How effective is corneal cross-linking (CXL) in treating keratoconus? Corneal cross-linking has a success rate of over 90% in halting the progression of keratoconus. It’s particularly effective in achieving long-term stabilisation of the condition in 85-95% of cases.
Q4. What happens during a corneal cross-linking procedure? The procedure involves applying riboflavin drops to the cornea and then exposing it to controlled ultraviolet light. This process typically takes 30-60 minutes and is performed as an outpatient treatment under local anaesthesia.
Q5. How long does it take to recover from keratoconus treatment? Recovery time varies, but vision typically begins improving within 3-4 days after treatment. However, full stabilisation can take 3-6 months. Patients usually experience significant improvement within 7-14 days, with vision continuing to stabilise over 2-3 months.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.
