Radial keratotomy was a popular surgical procedure that corrected myopia, and its effects continue to impact many patients today. About 10% of US ophthalmologists performed hundreds of thousands of RK procedures. The PERK study tracked results in 793 eyes at nine clinical centres. This “pizza pie surgery” has created long-term concerns as the central cornea flattens over time. Many patients become more longsighted (hyperopic) as a result.
Vision changes after radial keratotomy might make you wonder about laser vision correction options. Recent reviews show major improvements in uncorrected distance visual acuity through laser techniques. These include photorefractive keratectomy (PRK), topography-guided PRK, and wavefront-guided PRK. Traditional LASIK may not work best for post-RK eyes, but other approaches show promise. One clinical analysis found that 96% of treated eyes achieved 20/40 vision or better. Patients who aren’t good candidates for laser correction can still benefit from Custom Lens Exchange. This procedure replaces your natural lens with a custom implant.
Let’s explore all the vision correction possibilities available after radial keratotomy. You’ll learn what’s possible for your eyes’ unique situation.
Why Vision Changes After Radial Keratotomy Over Time
RK patients face ongoing challenges years after their original procedure. Medical professionals need to understand these changes to determine the right correction options.
Hyperopic Shift and Regression
Research shows a strong trend toward farsightedness in post-RK eyes over time. The Prospective Evaluation of Radial Keratotomy (PERK) study showed that 43% of RK-operated eyes developed a hyperopic shift of +1.00D or more during a ten-year follow-up period. This led to farsightedness in 36% of these eyes at the ten-year mark. The peripheral cornea’s elevation and central flattening cause this move.
Patients who had more extensive surgery to correct higher degrees of myopia experienced stronger hyperopic shifts. Studies also revealed that approximately 30% of eyes showed ongoing effects between one and three to four years after surgery. Researchers couldn’t predict when these changes would stop – or if they ever would.
Visual Disturbances: Glare, Halos, and Starbursts
RK patients often report visual issues that impact their daily activities. Light sources create starbursts at night when pupils dilate. RK incisions in the pupillary zone create surgical aberrations, including spherical aberrations, coma and trefoil, which cause these visual problems.
Brimonidine 0.15% can help troubled patients by shrinking their pupils by 1.0mm or more in dark conditions, which may reduce these disturbances. Vision quality changes throughout the day associate with normal intraocular pressure variations and might get worse from nighttime corneal swelling.
Age-Related Changes: Presbyopia and Cataracts
RK patients’ ageing process brings unique challenges with presbyopia and cataracts. These patients lose their ability to compensate for hyperopia along with normal age-related loss of accommodation. This makes it hard to see well both far and near.
Nuclear sclerosis affects post-RK eyes’ vision more than expected for the cataract’s size. RK-induced aberrations combine with early cataracts to create this effect. Cataract surgery becomes much more complex because of the unusual corneal shape with its flat centre and bulging edges. After cataract surgery, patients often experience temporary farsightedness from corneal swelling, but this usually improves with time.
Assessing Your Eyes for Further Treatment
A safe and effective treatment plan requires a full picture before any vision correction after radial keratotomy. Post-RK eyes need specialised review because of their unique characteristics, unlike standard vision correction cases.
Corneal Mapping and Biomechanical Analysis
Successful post-RK treatment depends on precise corneal mapping. Corneal tomography or scanning-slit interferometry delivers better results than standard topography. These technologies review both anterior and posterior corneal surfaces. This detailed analysis reveals the distinctive polygonal pattern often present in 59% of post-RK corneas.
Biomechanical assessment plays a vital role for post-RK eyes. The Corneal Visualisation Scheimpflug Technology (Corvis-ST) measures how corneas respond to air-puff deformation. It captures significant parameters like deformation amplitude, applanation time, and corneal stiffness. These measurements help doctors spot potential instability risks before additional laser treatment.
Ocular Surface Health and Tear Film Evaluation
Post-RK eyes often show poor tear film quality that affects vision stability. Lateral shearing interferometry reveals irregular interference fringes in post-RK corneas. Bright lines that show tear film breakups appear in predictable patterns.
A stable tear film matters greatly for accurate surgical planning. Interferometry studies confirm that post-RK corneal epithelium irregularities directly affect tear film instability. Doctors must complete a detailed dry eye review, including tear breakup time assessment, before making treatment decisions.
Determining Refractive Stability
Refractive stability must be established before any laser vision correction. Patient prescriptions should stay consistent for at least 3-6 months. This stability period confirms that the cornea has reached equilibrium after years of post-RK changes.
Measurements taken at different times of day provide reliable data. Post-RK eyes typically experience diurnal fluctuations averaging 0.39±0.07 diopters. Contact lens wearers need to stop using their lenses for 1-2 weeks before assessment to ensure accurate corneal measurements.
Had RK surgery years ago and now facing vision issues? Precision Vision London specialises in advanced solutions for complex cases like post-RK eyes. Book your consultation today to explore safe and effective laser or lens-based treatments designed for your unique vision needs.
What Laser Vision Correction Options Are Actually Possible?
Laser technology has evolved to provide several effective correction options for post-radial keratotomy patients who experience vision changes. New treatments can address many common complications, even decades after your original RK procedure.
Photorefractive Keratectomy (PRK) for Surface Treatment
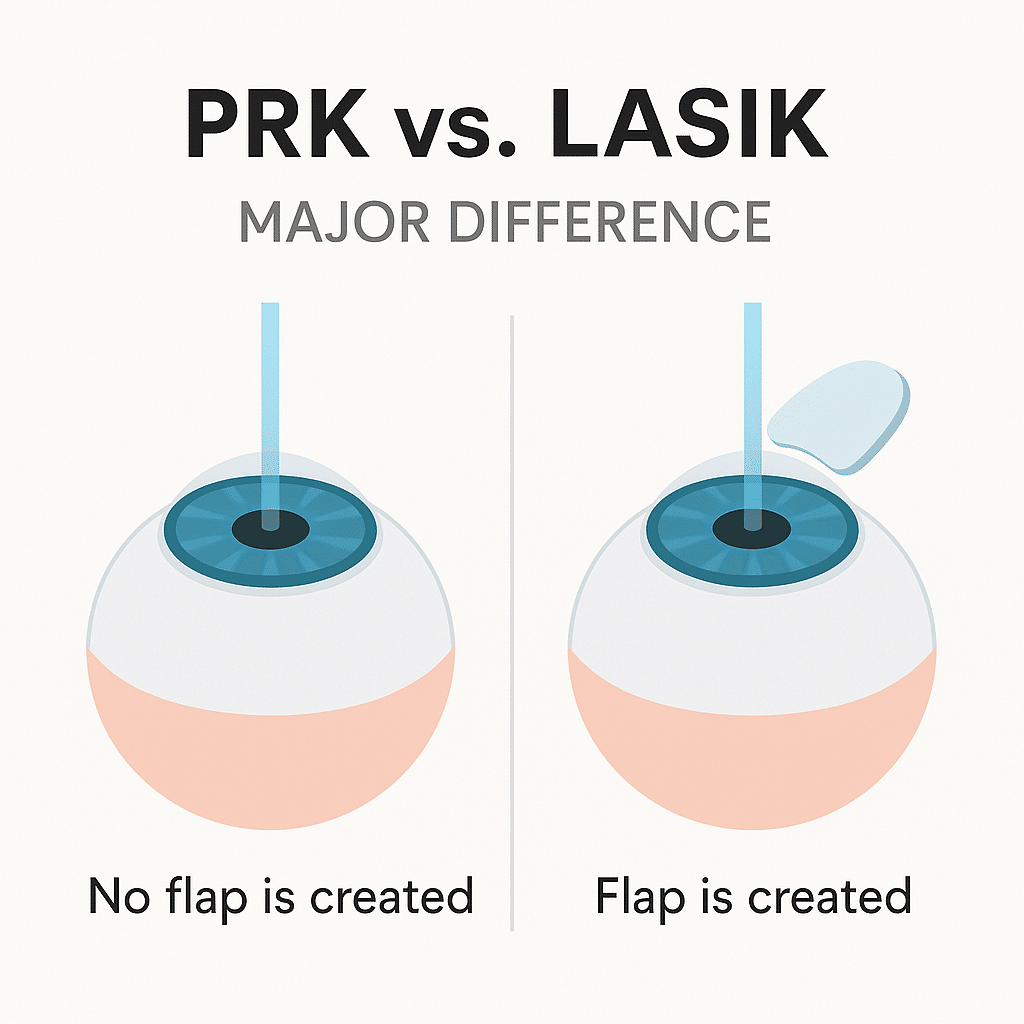
PRK is the life-blood of post-RK vision correction. PRK stands out from other approaches because it doesn’t create flaps that could weaken already compromised corneas. Studies demonstrate excellent PRK results after RK – no eyes lost their best-corrected visual acuity and approximately 33% gained one line of vision. The procedure requires careful de-epithelialization using alcohol or transepithelial approaches to protect incisions. The application of mitomycin C for 20-40 seconds helps prevent haze formation.
Topography-Guided Laser Eye Surgery for Irregularity
Topography-guided treatments are particularly effective at fixing irregular astigmatism that often occurs after RK. This method creates precise maps of each cornea’s unique height and curvature profiles to determine the ideal ablation pattern. Clinical studies show that topography-guided transepithelial PRK substantially improved both uncorrected and corrected distance visual acuity in post-RK patients. The technique reduced higher-order aberrations by 69% and improved vision-related quality of life scores in various areas.
Wavefront-Guided PRK for Higher-Order Aberrations
Wavefront-guided PRK targets specific visual aberrations caused by RK incisions. A multicentre study revealed this technique improved uncorrected visual acuity by an average of three lines. The results showed 56% of myopic eyes and 48% of hyperopic eyes achieved 20/20 vision or better. The study also found that 77% of treated eyes reached within ±0.25D of target refraction at three months.
Why LASIK May Not Be Ideal After Radial Keratotomy
LASIK’s popularity doesn’t make it the best choice for post-RK eyes. Major risks include potential flap fragmentation during manipulation and vertical gas breakthrough with femtosecond lasers. LASIK incisions must cut through existing RK incisions, which increases complications like epithelial ingrowth. PRK offers a safer option for cases with epithelial plugs in the incisions.
Had RK surgery years ago and now facing vision issues? Precision Vision London specialises in advanced solutions for complex cases like post-RK eyes. Book your consultation today to explore safe and budget-friendly laser or lens-based treatments designed for your unique vision.
When Laser Isn’t Enough: Other Vision Correction Options
Laser vision correction may not work well for some post-radial keratotomy patients. The good news is that other approaches can help with complex vision problems after RK surgery.
Refractive Lens Exchange for Ageing Lenses
Refractive Lens Exchange (RLE) works great for post-RK patients, especially when they’re over 50 and their lenses show age-related changes. The procedure swaps your natural lens with an artificial intraocular lens (IOL). This helps fix both refractive errors and early cataracts at the same time. RLE becomes particularly valuable when patients experience extreme hyperopic changes or don’t have enough corneal tissue to safely use lasers.
Custom Monovision or Multifocal IOLs
Advanced lens options exist for post-RK patients who don’t deal very well with presbyopia. Custom monovision setups can help you see at multiple distances by adjusting one eye for distance and one for near vision. Premium multifocal or extended depth of focus (EDOF) IOLs are another option that lets you see clearly at various distances without glasses. These advanced lenses balance the unique optical properties of post-RK corneas while tackling age-related presbyopia.
Corneal Cross-Linking to Halt Progression
Corneal cross-linking (CXL) can stabilise the eye when post-RK patients experience ongoing hyperopic changes or corneal instability. The procedure makes corneal tissue stronger by creating new bonds between collagen fibres, which stops progressive changes. CXL won’t directly improve vision but prevents further deterioration and creates a stable foundation for future vision correction procedures.
Personalised Treatment Planning at Precision Vision London
Post-RK eyes need unique treatment approaches at Precision Vision London. The planning process has detailed corneal analysis, lens assessment, and looks at your specific visual needs. This careful approach will give a clear picture of the best treatment option—whether laser-based or lens-based—for your situation.
Combination therapies often give better results for post-RK patients. To name just one example, your cornea might need stabilising with cross-linking first, followed by surface laser treatment or lens replacement later. Our expert surgeons use state-of-the-art technology and personalised care to prioritise safety while getting the best visual outcomes.
Conclusion
RK surgery creates unique challenges as patients age beyond their original procedure. Progressive hyperopic shift, visual disturbances, and age-related changes need specialised approaches to work well. Today’s patients can choose from several proven options to achieve clearer vision after RK surgery.
Surface treatments like PRK have shown remarkable success rates. Many patients experience better visual acuity without compromising their cornea’s integrity. Topography-guided treatments work well to address irregular astigmatism common in post-RK eyes. Wavefront-guided PRK targets the visual aberrations that RK incisions cause.
Excellent alternatives exist for patients who can’t have laser correction. Refractive Lens Exchange provides a complete solution, especially when you have age-related lens changes and RK-related vision issues. Corneal cross-linking helps stabilise progressing hyperopic shift and creates a foundation for future vision correction.
Your path to better vision needs a full picture from specialists who know post-RK eyes. Treatment decisions should reflect your cornea’s structure, tear film quality, and refractive stability. Precision Vision London combines advanced diagnostic technology with surgical expertise for complex cases like yours.
Clear vision remains possible after radial keratotomy. Advanced treatments can substantially improve your visual quality and reduce dependence on corrective eyewear, despite your original RK procedure’s challenges. Better vision begins with a complete consultation to find your best options. Our personalised care and advanced solutions can address your post-RK vision concerns and restore your clarity and confidence.
Key Takeaways
Post-radial keratotomy patients have several effective vision correction options available, despite the unique challenges their eyes present decades after the original procedure.
- PRK remains the safest laser option for post-RK eyes, avoiding flap complications whilst achieving impressive results with 33% of patients gaining vision lines.
- Topography-guided treatments excel at correcting irregular astigmatism, reducing higher-order aberrations by 69% and significantly improving quality of life.
- When laser correction isn’t suitable, Refractive Lens Exchange offers comprehensive solutions by replacing the natural lens with advanced IOLs.
- Thorough pre-treatment assessment is crucial, requiring corneal mapping, tear film evaluation, and 3-6 months of refractive stability confirmation.
- Combination therapies often yield superior results, such as corneal cross-linking to stabilise the cornea followed by targeted vision correction
The key to successful post-RK vision correction lies in personalised treatment planning that accounts for each eye’s unique characteristics, progressive changes, and individual visual needs.
FAQs
Q1. Is laser eye surgery possible after radial keratotomy? Yes, laser eye surgery is possible after radial keratotomy. Photorefractive Keratectomy (PRK) is generally considered the safest laser option for post-RK eyes. It avoids flap complications and has shown impressive results, with about 33% of patients gaining improved vision.
Q2. Can the effects of radial keratotomy be reversed or corrected? While the effects of radial keratotomy cannot be fully reversed, they can be corrected to a significant extent. Advanced techniques like LaZrPlastique® have been developed to safely correct vision in post-RK eyes, often achieving both distance and near vision without the need for glasses or contact lenses.
Q3. What are the latest advancements in laser eye surgery for post-RK patients? Recent advancements include topography-guided treatments, which excel at correcting irregular astigmatism common in post-RK eyes. These treatments can reduce higher-order aberrations by up to 69% and significantly improve vision-related quality of life.
Q4. How does LASIK compare to radial keratotomy? LASIK is generally considered superior to radial keratotomy (RK) in terms of precision, reduced scarring, and quicker healing. However, LASIK may not be ideal for post-RK eyes due to potential complications. PRK is often the preferred laser treatment for patients who have previously undergone RK.
Q5. What options are available when laser correction isn’t suitable for post-RK eyes? When laser correction isn’t suitable, alternatives like Refractive Lens Exchange (RLE) can be effective. RLE replaces the natural lens with an advanced intraocular lens, addressing both refractive errors and age-related lens changes. Corneal cross-linking is another option to stabilise the cornea and prevent further deterioration.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

