People with keratoconus face a higher risk of developing cataracts earlier in life than others. This creates a special challenge because keratoconus affects the cornea and leads to worse vision in young people.
Vision problems from both conditions make understanding cataract surgery‘s effect on keratoconus vital. The surgery brings back clear vision by taking out the cloudy natural lens and putting in a clear artificial intraocular lens (IOL). But doctors find it hard to predict how well keratoconus patients will see after surgery, even with careful planning beforehand. New developments give hope to better results. These include special IOL formulas made for keratoconus and better lens technology.
Our clinic knows how complex it is to treat both conditions together. This piece answers the question “can cataract surgery help keratoconus?” We look at evidence from UK clinics and identify patients who benefit most. We also explain custom surgical approaches that work best. The question about cataract surgery’s effect on keratoconus progression comes up often. Our team’s experience with these challenging cases helps us give you a clear picture.
Why Cataract Surgery Matters in Keratoconus Management
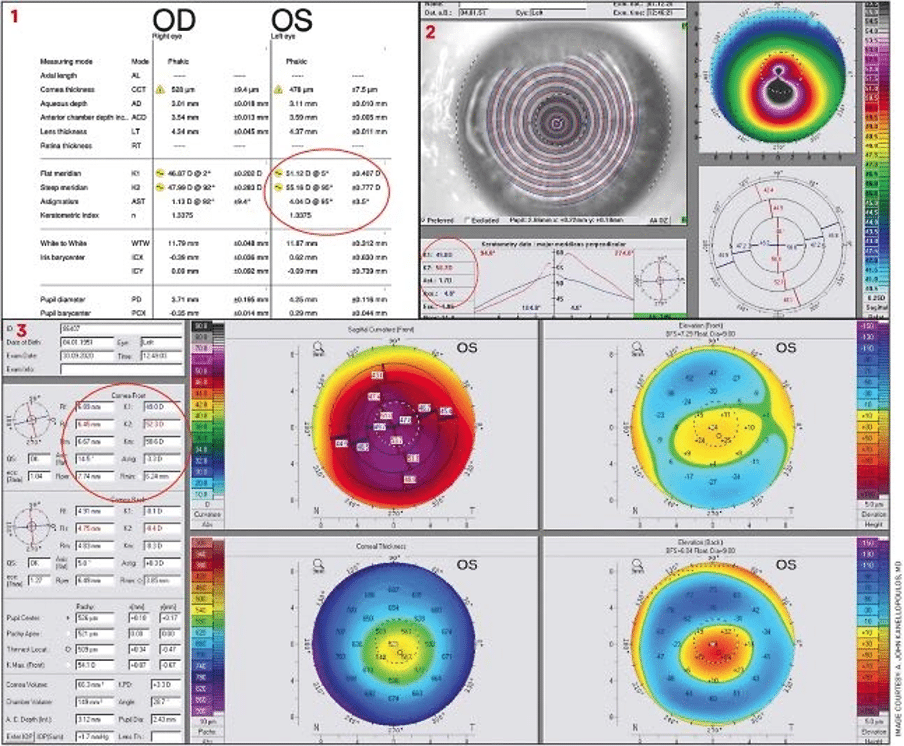
Image Source: Ophthalmology Management
Cataracts and keratoconus create unique challenges for eye surgeons. These conditions affect vision differently, and patients with both conditions need special care.
Can cataract surgery help keratoconus? Evidence from UK clinics
London patients has shown promising results about cataract surgery in keratoconus. Patients with mild keratoconus (K<48D) showed great results – 60% reached within ±1D of their target vision. UK clinical data shows even better results, with about 75% of keratoconus patients reaching within 1D of their target after surgery.
Vision improvements can be remarkable. Research shows that lens replacement surgery boosted best corrected visual acuity (BCVA) no matter how severe the keratoconus was. Patients gained about 4 lines of better vision. Perfect vision might not happen for everyone, but patients definitely see better after surgery.
Results vary by a lot based on how severe the disease is. Eyes with more irregular corneas make surgical results harder to predict. A patient with moderate keratoconus might end up with vision anywhere from +3.2D to -3.8D different than planned. This shows how tricky it can be to get exact results in more serious cases.
Visual decline from lens opacity vs corneal distortion
Doctors must figure out what’s causing the main vision problems in keratoconus patients who have cataracts. Both conditions hurt vision differently, and knowing which one is the bigger problem helps choose the right treatment. Proteins in the lens break down to form cataracts, which create cloudy spots that get worse over time. Keratoconus works differently – the cornea gets thinner and bulges out. These conditions can look similar, so doctors need to tell them apart carefully.
Modern imaging helps doctors tell these conditions apart. Corneal topography shows the front curve of the cornea, and Scheimpflug imaging gives detailed pictures of both front and back corneal surfaces. These tools help doctors learn whether cloudy lenses or distorted corneas cause the vision problems. Research shows an interesting link between certain types of lens cloudiness and keratoconus. One study found that almost all patients (95.2%) with unusual lens cloudiness had keratoconus. People with keratoconus tend to get cataracts younger, and nuclear sclerosis shows up most often (83%).
How cataract surgery can unmask or stabilise keratoconus
Sometimes cataract surgery reveals hidden keratoconus. After removing the cloudy lens, irregular corneas become the main vision problem. This might change how well glasses work or make vision less clear than expected after surgery. Stable keratoconus usually doesn’t get worse after cataract surgery. Most cases stabilise by age 30, and progression rarely happens after 50. Older patients with known keratoconus usually lose vision because of cataracts, not worsening corneal problems.
Doctors check if keratoconus is stable through repeated cornea scans before cataract surgery. Active progression needs corneal cross-linking before lens surgery. Doctors watch the eyes for 3-6 months after cross-linking to make sure the cornea stays stable before doing lens surgery. Cataract surgery won’t fix corneal irregularity from keratoconus, but it helps vision by fixing lens problems. Most patients see better after surgery, even if they still need contact lenses to see their best.
Patient Profiles That Benefit Most from Surgery

Image Source: Cataract & Refractive Surgery Today
Doctors need to carefully assess which patients with keratoconus should get cataract surgery. Not all patients will see the same benefits from this procedure. A full picture of patient profiles helps set realistic expectations and leads to better surgical outcomes.
Mild keratoconus with good spectacle correction
Patients who have mild to moderate stable keratoconus and see well with glasses before cataracts develop tend to get excellent results. These patients usually have clear central corneas and show regular astigmatism patterns where the steep and flat axes are about 90 degrees apart. Research shows that mild keratoconus cases do well after cataract surgery. A clinical study found that two patients no longer needed glasses after surgery, and two others switched from rigid gas permeable lenses to soft toric contact lenses. This change made their lives much better.
Your dependence on corrective lenses might decrease if you have mild keratoconus with regular corneal astigmatism patterns. If you have keratoconus and cataracts, speak to our experts at Precision Vision London to explore how surgery could improve both vision and quality of life.
Advanced keratoconus with contact lens intolerance
Cataract surgery can be especially helpful for patients who have moderate to severe keratoconus and can’t wear rigid gas permeable or scleral lenses. Research shows that doctors diagnose approximately 25% of keratoconus patients after age 50. Many develop cataracts earlier than others.
Patients who struggle with contact lenses have few options to improve their vision. Cataract surgery gives them a chance to:
- Reduce overall refractive error
- Improve uncorrected visual acuity
- Better handle simpler optical corrections
A UK study revealed that among patients with moderate keratoconus who had cataract surgery, five out of seven eyes could wear the same contact lenses they used before surgery. This shows that corneal shape stays stable during and after cataract removal.
Post-crosslinking patients with stable topography
Patients who have had corneal cross-linking (CXL) make great candidates for cataract surgery once enough time passes to confirm stability. CXL stops keratoconus from getting worse and creates a more predictable corneal surface for surgery planning. The best results come from completing CXL before cataract surgery for progressive keratoconus patients who still see well with glasses or contact lenses. Regular topography measurements must show stable keratoconus before moving forward with lens extraction.
Doctors should monitor patients for 3-6 months after cross-linking to confirm stable keratometric readings before cataract surgery. This waiting period helps achieve predictable results and reduces unexpected outcomes.
Some post-CXL patients with stable corneas might qualify for toric intraocular lenses. This works best for those who see well with glasses, have low higher-order aberrations, and likely won’t need corneal transplants. The timing between stabilising keratoconus and performing cataract surgery plays a crucial role in visual results. Getting these steps in the right order leads to success with these challenging cases.
Customised Surgical Approaches for Better Results
Your surgical approach needs customisation to treat both cataracts and keratoconus. Surgeons can now tailor procedures based on your cornea’s unique characteristics through advanced techniques.
Using toric IOLs when astigmatism axis is stable
Toric intraocular lenses show promising results for some keratoconus patients, but careful evaluation is necessary. The best candidates have mild to moderate (stage I or II) keratoconus with regular to slightly irregular astigmatism and stable corneal topography. Research shows that postoperative spherical equivalent correction falls within ±1D of target in 95% of eyes with mild keratoconus receiving toric IOLs.
Doctors used to avoid premium lens technologies in keratoconus cases. Clinical experience now shows that carefully chosen patients get exceptional benefits. A case series revealed that 90% of patients with mild keratoconus who received toric IOLs didn’t need contact lenses after surgery.
Our specialists ensure success with toric IOLs by checking:
- Stability through multiple consecutive topography examinations
- Regular astigmatism pattern with identifiable major axis
- No predicted need for corneal transplantation
Sequential ICRS and cataract surgery in irregular corneas
Patients with irregular corneal surfaces often get better results from a two-step approach. This involves using intrastromal corneal ring segments (ICRS) first, followed by cataract surgery. The cornea becomes more regular before lens extraction, which creates a more predictable optical system.
Clinical studies prove this method works well. One patient’s central keratometry dropped from 60D to 55D after femtosecond-assisted Keraring implantation and cataract surgery three months later. Their spectacle-corrected visual acuity improved to 20/25. A larger study looked at sequential Ferrara ICRS and IOL implantation with six-month gaps between procedures. The results showed good visual outcomes in 47 of 70 eyes over five years.
Triple procedure: cataract surgery with keratoplasty
Advanced keratoconus patients with significant corneal opacity benefit from a triple procedure. This combines penetrating keratoplasty (PK), cataract extraction, and IOL implantation. The approach reduces endothelial damage risk by avoiding multiple surgeries.
Our surgeons at Precision Vision London achieve great results with this method. Studies show best-corrected visual acuity improves by 10 lines on the Snellen chart. About 40.8% of eyes achieve vision of 20/40 or better. Graft survival rates after triple procedures range from 60% to 100%. Keratoconus patients show better results compared to other conditions.
The triple procedure’s refractive predictability remains challenging. Only 46.05% of eyes achieve postoperative spherical equivalent within ±2.0D of target. Yet it remains a great option for suitable candidates with combined pathology.
Visual Outcomes and Refractive Accuracy
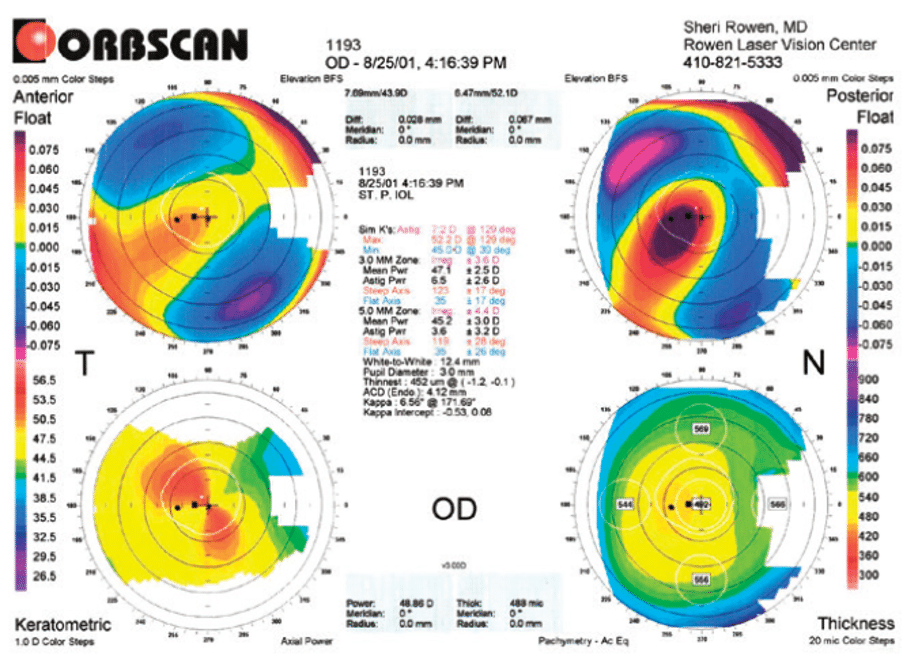
Image Source: Cataract & Refractive Surgery Today
Patients with keratoconus show different levels of refractive accuracy after cataract surgery. This knowledge helps patients and doctors set the right expectations before surgery.
UK-based outcomes: 75% within 1D of target refraction
Clinical data from the UK shows that about 75% of keratoconus patients reach a refractive outcome within 1D of target after cataract surgery. The original results show 50% end up within 0.5D of planned refraction—much lower than the 80-90% success rate in healthy eyes. Results become less predictable as keratoconus gets worse. Research points to hyperopic prediction errors in keratoconic eyes, and accuracy drops as the disease becomes more severe.
Mild keratoconus cases (mean K<48D) get better results when doctors use actual K values with a low myopia target (-1.0D). This approach helps 60% of patients reach within 1D of target. However, severe keratoconus cases using measured K values can lead to hyperopic error, sometimes exceeding +6D.
Postoperative UDVA improvements by keratoconus stage
Each stage of keratoconus shows different visual improvements. Mild cases usually see uncorrected distance visual acuity (UDVA) improve from 0.5 logMAR (20/60) to 0.2 logMAR (20/30). These patients often don’t need glasses or can switch from rigid to soft toric lenses.
Moderate keratoconus shows smaller gains, while severe cases see dramatic improvements—from preoperative UDVA of 1.34 logMAR (20/440) to postoperative 0.57 logMAR (20/75). The average corrected distance visual acuity improves to about 0.2 logMAR across all stages.
Residual ametropia correction with TICL or spectacles
Leftover refractive error happens often, despite surgical precision. Here are effective ways to manage this:
- Spectacle correction: Works well for mild residual error, especially in mild keratoconus
- Contact lenses: Options range from soft toric lenses for mild irregularity to RGP lenses for higher error
- Toric Implantable Collamer Lens (TICL): This works really well to correct remaining astigmatism. Patients achieve UDVA of 0.1-0.3 logMAR (20/25-20/40) with minimal residual cylinder
Our team at Precision Vision London talks about these options before surgery. We make sure you know you might need correction afterward. Our experts know how to manage residual error with the right solution for your specific vision needs.
Long-Term Benefits and Patient Satisfaction
Cataract surgery gives keratoconus patients lasting benefits that boost their quality of life beyond just better vision.
Improved visual function in daily life
Research shows cataract surgery makes a real difference in how keratoconus patients see and function. Studies highlight these improvements:
- Aided visual acuity, with an average gain of 4 lines of vision
- Better contrast sensitivity and depth perception within 3 months after surgery
- Less disability glare that no longer affects how well patients see
These improvements make daily life much easier. Vision-specific health scores show better results throughout recovery. Patients find it easier to read, drive, and recognise faces—tasks that challenge many keratoconus patients.
Reduced need for corneal transplant in some cases
Cataract surgery helps many patients avoid or postpone more complex corneal procedures. About 20% of keratoconus patients typically need corneal transplantation during their lifetime. Modern cataract surgery techniques have reduced this number.
Clinical evidence shows many patients see well enough after cataract surgery that they don’t need corneal transplants. One key study found patients developed good vision with just cataract surgery, and none chose to get corneal transplants afterward.
Our experts at Precision Vision London can help you learn how surgery could boost your vision and quality of life if you have keratoconus and cataracts.
Does cataract surgery help keratoconus progression?
Here’s what you need to know: cataract surgery doesn’t make keratoconus better or worse. Your corneal condition and cloudy lens are separate issues that need different treatments.
Patients with unstable keratoconus get the best results from a two-step approach. We first use corneal collagen cross-linking (CXL) and then perform cataract surgery. Cross-linking stops progression in about 98% of cases. This locks in your corneal shape before we fix the cloudy lens.
We check your keratoconus stability through repeated topography measurements before suggesting cataract surgery. This careful approach ensures your corneal condition stays stable while we address your cataract-related vision problems.
Conclusion
Cataract surgery is a chance for keratoconus patients to see better than they ever could with contact lenses or glasses. In this piece, we’ve seen strong evidence from UK clinics that shows about 75% of keratoconus patients get refractive outcomes within 1D of their target after surgery. On top of that, patients usually see four lines better on the vision chart, which makes a big difference in their daily life and how well they can see.
Your results will mostly depend on how severe your keratoconus is. Mild cases get the most predictable results. Whatever the severity, the benefits go beyond just seeing better right away. Many patients don’t need to rely so much on rigid contact lenses. Some even avoid corneal transplants or push them further down the road.
Picking the right patients is key to getting good results. People who do best with cataract surgery include those with mild keratoconus and good glasses correction, advanced cases where contact lenses don’t work anymore, or patients with stable topography after crosslinking. At Precision Vision London, we offer custom surgical approaches. These include toric IOLs for stable astigmatism, sequential ICRS procedures, or triple procedures that combine keratoplasty. Each plan targets your specific vision needs.
Perfect vision might not be possible for everyone, but better vision definitely is. After surgery, options like glasses, contact lenses, or toric implantable collamer lenses help fix any remaining vision problems and get you the best possible results.
Without doubt, deciding to have cataract surgery when you have keratoconus needs expert evaluation and realistic expectations. Our specialists at Precision Vision London use advanced diagnostic tech and bring years of experience to figure out if this life-changing procedure might help you. Bringing back clear vision through cataract removal while working around keratoconus is one of modern ophthalmology’s most rewarding challenges.
FAQs
Q1. Can cataract surgery improve vision for keratoconus patients? Yes, cataract surgery can significantly improve vision in patients with keratoconus. Studies show that patients often gain an average of 4 lines of vision after surgery, with improvements in best-corrected visual acuity across all severities of keratoconus.
Q2. What type of intraocular lens is recommended for keratoconus patients undergoing cataract surgery? For mild and stable keratoconus, toric intraocular lenses (IOLs) may be suitable. However, monofocal IOLs are generally a better choice for patients with advanced keratoconus. The selection depends on the individual’s corneal stability and astigmatism pattern.
Q3. How does cataract surgery affect keratoconus progression? Cataract surgery itself neither worsens nor improves keratoconus progression. For patients with unstable keratoconus, a two-stage procedure combining corneal collagen cross-linking (CXL) to stabilise the cornea, followed by cataract surgery, often provides optimal results.
Q4. What are the long-term benefits of cataract surgery for keratoconus patients? Long-term benefits include improved visual function in daily life, enhanced contrast sensitivity, and reduced disability glare. Some patients may also avoid or delay the need for corneal transplantation. Many experience reduced dependency on rigid contact lenses post-surgery.
Q5. What percentage of keratoconus patients achieve their target refraction after cataract surgery? According to UK clinical data, approximately 75% of keratoconus patients achieve a refractive outcome within 1 dioptre (D) of the target after cataract surgery. However, the predictability decreases as keratoconus severity increases.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

