Topography-guided laser technology has changed astigmatism treatments and now provides better precision and visual outcomes. Research shows that 93% of eyes achieve 20/20 or better uncorrected distance visual acuity after these custom treatments. The results are impressive as 30% of patients see better after surgery than they did with glasses or contact lenses.
Topography-guided treatments offer a customised solution that matches your unique eye shape perfectly if standard laser eye surgery isn’t right for you. This advanced method delivers great results – 65% of patients have improved best-corrected visual acuity. Patients with astigmatism see their cylindrical error reduce by a lot, dropping from -3.91D to -1.45D on average. Our expert surgeons at Precision Vision London use advanced diagnostic imaging and software-assisted planning tools like Phorcides. This system shows better outcomes with the lowest mean error vector magnitude (0.26D) compared to other approaches.
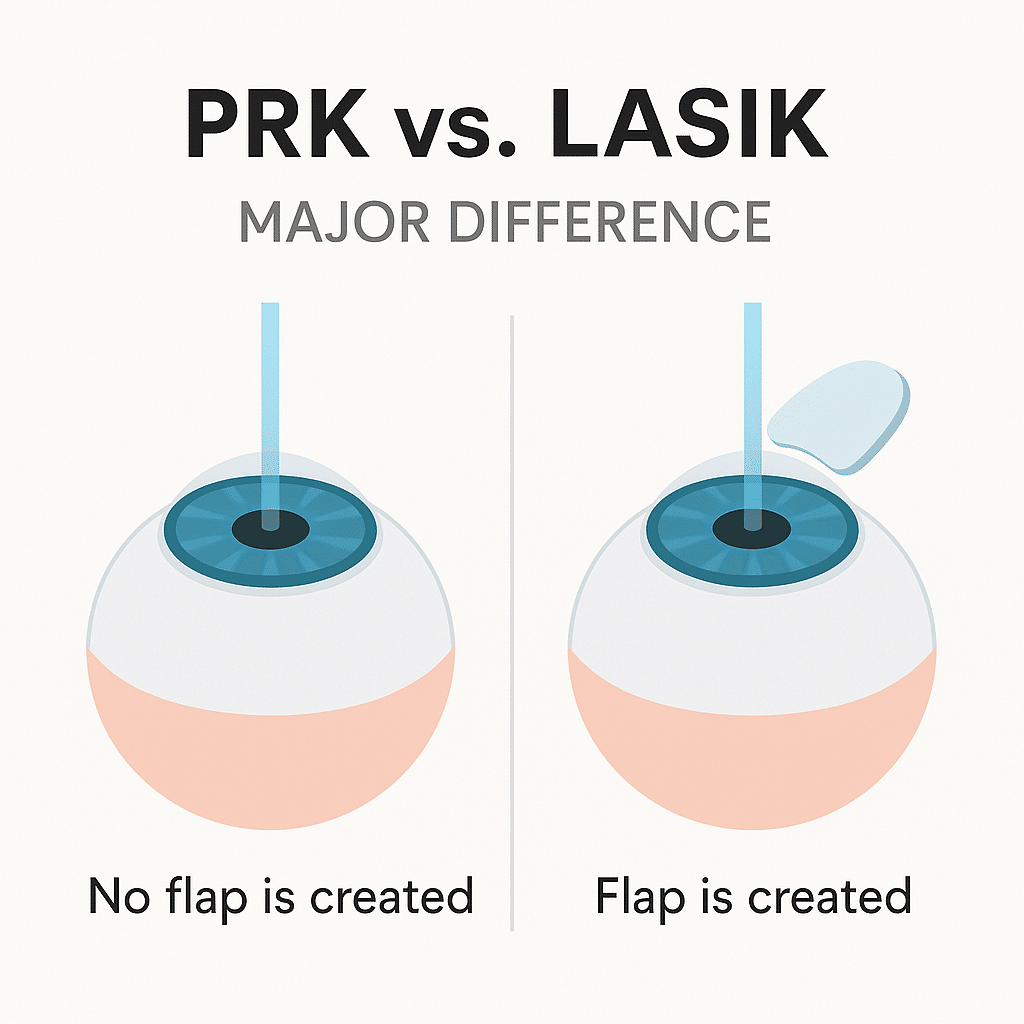
This piece explains how topography-guided laser treatments including LASIK and PRK can improve your vision if you have astigmatism or irregular corneas. You’ll find out who makes a good candidate, what happens during treatment, and the amazing results our patients get through our all-encompassing approach to care.

Who Can Benefit from Topography-Guided Laser Eye Surgery
Topography-guided laser treatments are a great way to help patients whose corneal irregularities make them poor candidates for standard laser vision correction. This advanced technique reshapes the cornea into a more regular surface. The treatment helps fix complex visual problems that regular glasses or contact lenses can’t correct.
Patients with irregular astigmatism
Standard ablation techniques don’t deal very well with the unique challenges of irregular astigmatism. Regular laser procedures mainly fix low-order aberrations like defocus and regular astigmatism. These treatments become less effective when dealing with irregular corneal surfaces. Topography-guided treatments shine in these cases. Studies show improved best-corrected visual acuity in 65% of patients with irregular corneal surfaces.
This approach works best for patients who still have vision problems even with the right prescription. Some common signs of irregular astigmatism are:
- Visual distortion and reduced clarity
- Glare and halos, especially in dim light
- Monocular diplopia (double vision in one eye)
- Poor contrast sensitivity
Our advanced corneal imaging systems at Precision Vision London can spot even tiny corneal irregularities causing these symptoms. Topography-guided treatment is especially valuable because it fixes anatomical rather than physiological changes. This makes it more reliable than wavefront-guided laser ablation when dealing with intraocular factors.
Mild keratoconus and early ectasia
Early treatment with topography-guided procedures shows excellent results for patients with mild keratoconus. This condition usually affects younger patients until they reach about 30. It causes uneven corneal steepening and increases myopic and astigmatic errors.
Patients under 35 with new keratoconus diagnoses can benefit from topography-guided PRK combined with corneal collagen cross-linking (CXL). This combination stops disease progression and improves vision. The procedure remains stable for up to 30 months after treatment. It reduces corneal irregularity and visual symptoms without losing best-corrected visual acuity. Most patients see better vision afterward.
The best candidates should have corneal thickness of at least 400µm at the thinnest point after treatment. Results are ideal when there’s less than 10D difference across the cornea within a 6mm optical zone. Patients over 40 might only need topography-guided PRK without cross-linking since natural corneal cross-linking happens with age.
Post-refractive surgery complications
Topography-guided treatments help patients who have vision problems after previous laser eye surgery. These issues include:
- Decentered ablations: Modern eye-tracking technology makes these rare now. But when decentration goes beyond 1.0mm, it can cause major vision problems. Research shows topography-guided treatment improves both uncorrected and corrected visual acuity for these patients.
- Small optical zones: Earlier laser systems used smaller optical zones to reduce stromal ablation, especially for high myopia corrections. This often led to night vision problems like halos and glare. Topography-guided treatments can make these zones larger and smoother, which reduces symptoms.
- Post-LASIK ectasia: Using topography-guided ablation with corneal cross-linking works well for iatrogenic ectasia after LASIK. This stops the condition from getting worse and keeps refraction and topography stable.
At Precision Vision London, we use multiple topographic screening tools and epithelial mapping to create custom treatment plans. Complete visual recovery can take up to three months. Most patients see daily improvements, and younger patients usually get normal epithelium back within five days.

Diagnostic Imaging and Preoperative Assessment
Successful topography-guided laser treatments rely on accurate diagnostic imaging. Precision Vision London creates personalised treatment plans based on a detailed preoperative assessment. Our team identifies how corneal irregularities affect your vision.
Corneal topography and tomography
Your preoperative evaluation for laser vision correction must include corneal topography. This advanced mapping technology measures your cornea’s shape and curvature. Abnormal corneal topography stands out as the biggest identifiable risk factor for corneal ectasia.
Traditional topographers (first-generation devices) use Placido disc technology to check only the front corneal surface. Modern tomography systems now provide complete three-dimensional analysis. These advanced instruments measure both anterior and posterior corneal surfaces through direct measurements instead of mathematical assessments.
Our clinic uses multiple imaging systems to get a full picture:
- Placido disc-based topographers to map front surface in detail
- Scheimpflug rotating camera technology for full corneal analysis
- Combined systems like Galilei® and Sirius® that merge multiple technologies to improve accuracy
These systems measure SimK (simulated keratometry) values with precision for patients with astigmatism. Normal eyes show a mean astigmatism of 0.90 dioptres. Different topographic patterns help us spot irregularities that might affect your treatment plan.
Epithelial mapping with OCT
The corneal epithelium (outer layer) naturally reshapes itself to balance underlying irregularities. This “masking effect” can hide early signs of conditions like keratoconus. OCT epithelial mapping shows these subtle changes that might go unnoticed otherwise.
Healthy eyes maintain uniform epithelial thickness. The central cornea measures an average of 45.7 μm at the corneal vertex. Keratoconus creates a distinctive “donut pattern” with central thinning (as low as 38.2 μm) surrounded by thickened epithelium (up to 66.8 μm). Our advanced OCT imaging spots these patterns accurately. Studies using this technology are great at telling keratoconic corneas from normal ones – with 99.5% specificity and 98.9% sensitivity. This precision helps us assess suitability for astigmatism correction by detecting early ectasia that might rule out certain procedures.
Assessing corneal thickness and cone location
Corneal thickness measurement determines treatment eligibility. Our detailed pachymetry maps find your cornea’s thinnest point. This point averages 0.55 mm in thickness and sits about 0.90 mm from the visual axis. The thinnest point’s location provides vital information for patients with irregular astigmatism or mild keratoconus. Normal eyes show this point in the inferotemporal quadrant 69.57% of the time. Any shift from this position often signals irregularity that needs special attention.
Topography-guided treatments require these minimum corneal thickness values:
- At least 450 μm preoperatively at the thinnest point
- A predicted postoperative thickness of at least 400 μm
The cone’s location in keratoconus affects treatment planning significantly. Our surgeons check if the cone sits within or outside the central 2-mm zone. This difference shapes both treatment approach and expected outcomes.
Precision Vision London combines advanced diagnostic technologies with surgical expertise to create custom treatment plans. We understand your unique corneal characteristics to choose the best approach – LASIK, PRK, or transepithelial PRK. This helps us deliver optimal visual outcomes for your specific type of astigmatism or corneal irregularity.
Treatment Options: LASIK, PRK, and Transepithelial PRK
Patients with astigmatism or irregular corneas need the right laser procedure based on their corneal characteristics, visual requirements, and lifestyle. Topography-guided treatments give better results in procedures of all types, each offering unique benefits for specific corneal conditions.
Choosing between LASIK and PRK for astigmatism
Your choice between LASIK and PRK to correct astigmatism depends on your corneal thickness, irregularity level, and risk factors. LASIK creates a corneal flap before reshaping with laser and gives you faster visual recovery with less discomfort. Research shows LASIK helps patients with irregular astigmatism improve their uncorrected visual acuity from 20/100 to 20/40 on average.
PRK works differently by removing the epithelium completely before treatment. This makes it ideal for patients with thinner corneas or mild surface irregularities. Studies show PRK helps improve uncorrected visual acuity from 20/60 to 20/40 and reduces refractive cylinder from -2.25D to -1.5D.
These factors help determine the best choice:
- Corneal thickness – PRK becomes necessary for thinner corneas (below 500μm)
- Recovery expectations – You’ll recover vision faster with LASIK (24-48 hours) compared to PRK (5-7 days)
- Occupation and lifestyle – PRK suits you better if you play contact sports or do high-impact activities since there’s no flap risk
- Previous corneal conditions – You’ll need PRK if you have epithelial basement membrane disorders
Our surgeons at Precision Vision London assess these factors along with topographic data to recommend your best option. PRK often works better for higher degrees of irregular astigmatism because it treats the entire corneal surface without flap-related restrictions.
When is trans-PRK preferred?
Transepithelial PRK (trans-PRK) represents the latest advancement in standard PRK. The laser treats both epithelium and stroma in one continuous session. This “no-touch” approach works better in specific astigmatism cases. Trans-PRK excels at precise epithelial removal, especially in post-radial keratotomy irregularities. Patients saw their uncorrected distance visual acuity improve from 0.45 LogMAR to 0.25 LogMAR after six months. The technique also improved corrected distance visual acuity from 0.14 LogMAR to 0.09 LogMAR.
This technique works best for:
- Patients with severe irregular astigmatism after penetrating keratoplasty. Studies show major improvements in vision metrics and reduced spherical equivalent from -3.75D to -1.60D.
- Corneas with difficult surface features where mechanical epithelial removal might cause more irregularity.
- Cases needing exact epithelial ablation profiles based on OCT epithelial mapping.
Trans-PRK’s single-step nature keeps corneal hydration stable and reduces treatment time. The natural shape of your corneal surface stays preserved throughout the procedure. The stromal ablation starts right after epithelial removal, maintaining ideal hydration for more predictable results.
Role of mitomycin C in haze prevention
Corneal haze can occur after surface ablation treatments, especially in patients needing higher corrections or those with irregular astigmatism. Mitomycin C (MMC), an antifibrotic agent, helps minimise this risk. MMC stops fibroblast growth and collagen synthesis that leads to haze. Doctors apply a dilute solution (usually 0.02%) for 30-60 seconds after laser treatment to prevent scarring below the epithelium while maintaining good vision.
Research proves MMC works well. A study of eyes with irregular astigmatism after radial keratotomy found zero cases of significant haze (greater than grade 1) with MMC treatment, while 63% of untreated eyes developed haze. The American Society of Cataract and Refractive Surgery reports 88% of surgeons now use MMC routinely to prevent corneal haze.
The treatment follows these steps:
- Cool the cornea with frozen balanced salt solution for 10 seconds after ablation
- Apply MMC with a soaked disc for 40-60 seconds
- Rinse thoroughly to remove all MMC from the eye’s surface
Long-term safety research confirms MMC doesn’t affect endothelial cell density when used correctly. This proves its safety for astigmatism treatments when experienced surgeons perform the procedure.
Customising the Laser Plan for Each Eye
Successful topography-guided treatments for astigmatism depend on tailoring the laser plan to each eye’s unique features. Your visual experience comes from the interaction of different measurements that need sophisticated analysis.
Using manifest vs topographic cylinder
Doctors face a key challenge when planning astigmatism treatments. They must balance two often different measurements: manifest refractive astigmatism (what you experience subjectively) and anterior corneal topographic astigmatism (measured objectively). This difference, known as ocular residual astigmatism (ORA), comes from factors like posterior corneal astigmatism, lenticular astigmatism, and higher-order aberrations.
With-the-rule astigmatism shows lower refractive than corneal astigmatism. Against-the-rule astigmatism shows greater refractive than corneal astigmatism. Posterior corneal influences create this relationship.
Our surgeons look at these factors to decide which measurement matters most:
- How much the measurements differ
- Astigmatism’s direction and axis
- Higher-order aberrations present
- Patient’s specific visual needs
Research shows that manifest refraction-based planning delivers excellent results. A largest longitudinal study of 25,396 eyes found that even large discrepancies (45° to 90°) between refractive and topographic measurements produced similar visual outcomes compared to eyes with slight differences.
Adjusting for angle and power discrepancies
Significant differences between manifest and topographic measurements need strategic adjustments. Several methods have emerged:
- Topography-modified refraction (TMR) blends clinical refraction with topographic data. This method combines corneal astigmatic power and axis from topography with manifest refraction to optimise treatment planning. Studies show TMR left residual refractive astigmatism over 0.5D in just 11.7% of eyes compared to 27.8% in the manifest refraction group.
- Dr. Wexler’s “50/50 method” uses 50% of the difference between manifest and topographic measurements with the topographic axis. This approach rarely “flips” an astigmatic axis but may leave some untreated astigmatism.
- Complex cases with highly irregular corneas might need partial refractive correction based on spherical equivalent and pachymetry. Corneas with spherical equivalent <6D and thinnest pachymetry >475 μm can usually receive partial refractive treatment that preserves corneal integrity.
Software-assisted planning with Phorcides
Phorcides Analytic Engine has transformed advanced treatment planning through mathematical analysis that removes subjective decisions. This software:
- Analyses anterior topographic profile through geographic imaging technology
- Includes posterior corneal astigmatism and internal (lenticular) astigmatism
- Employs vector analysis to determine optical effects of removing topographic irregularities
- Creates treatments based on individual eye data instead of averaged results
Results prove its effectiveness. Clinical studies show remarkable outcomes three months after treatment. All eyes achieved 20/20 uncorrected visual acuity. Most patients (89%) reached 20/15 or better, while 28% achieved 20/12.5 or better. Better still, 92% of eyes had postoperative uncorrected vision matching or exceeding their preoperative corrected vision. Patient experience showed notable improvements. They reported much less glare, halos, night driving difficulties, reading problems, starbursts, vision fluctuation, and light sensitivity.
Precision Vision London’s surgeons create truly personalised treatment plans. We analyse both manifest and topographic measurements with advanced planning software. This helps optimise outcomes for all patients, even those with major differences between their subjective experience and objective measurements.

Precision Vision London’s Approach to Personalised Care
Precision Vision London starts your personalised care before your first consultation. We blend clinical expertise with innovative technology to treat astigmatism and irregular corneas. Our results often go beyond what patients expect.
Consultation and patient education process
Your experience at Precision Vision London begins with a complete consultation to learn about your specific visual needs. We spend 90-120 minutes to get a full picture of your visual system. Our specialists will:
- Learn about your lifestyle needs and vision goals
- Look at your eye history and past treatments
- Check your vision with and without correction
- Show you how astigmatism affects your eyesight
Patient education is the life-blood of our approach. We use detailed visual aids and 3D models to show you your cornea’s unique shape. You’ll see how topography-guided treatments can fix your astigmatism. Standard consultations just focus on measurements. We make sure you understand all your treatment options.
Advanced diagnostic equipment used in clinic
The success of astigmatism treatment depends on quality diagnostic information. Precision Vision London has invested in state-of-the-art technologies:
- Our Scheimpflug imaging systems map your cornea in 3D. These maps show front and back surface irregularities that might cause your astigmatism. High-resolution OCT epithelial mapping spots subtle corneal changes that regular topography might miss.
- Patients with irregular astigmatism or mild keratoconus benefit from our wavefront aberrometry. This technology measures higher-order aberrations affecting night vision and contrast sensitivity. It finds visual disturbances that standard prescriptions can’t detect.
These diagnostic systems work together to give our surgeons unmatched information about your visual system. Each measurement helps build a complete map of your eye’s optical characteristics.
Tailored treatment plans by expert surgeons
Our surgeons analyse your diagnostic data using advanced software platforms like Phorcides and proprietary algorithms. These tools help settle any differences between how you experience astigmatism and what we measure.
Our unique approach comes from personalising every part of your treatment plan. We look at:
- The best mix of topographic and refractive data for your corneal pattern
- Which procedure – LASIK, PRK, or transepithelial PRK – will work best for your cornea
- The exact treatment zone size based on your pupil size and corneal irregularity
- Custom laser settings that match your corneal tissue
Our surgeons specialise in complex astigmatism cases and have extensive experience with irregular corneas. They often achieve vision without correction that’s better than what patients had with glasses or contacts. This integrated approach combines detailed consultation, advanced diagnostics, and expert surgical planning. We create treatment plans that are as unique as your eyes to give you the best possible vision and safety outcomes.
Expected Results and Visual Recovery Timeline
Patients who undergo topography-guided laser treatment for astigmatism see remarkable improvements in their vision quality. Recovery times vary based on the type of treatment and individual factors. This piece will help you understand what to expect during your recovery experience after surgery.
Visual acuity improvements by day and week
The visual results from topography-guided treatments unfold gradually after surgery. LASIK patients recover faster than PRK patients. Studies show 63% of topography-guided LASIK patients get 20/16 vision or better just one day after surgery. This number jumps to 89% by the end of week one. PRK recovery works differently. The surface layer of cells needs about 3-5 days to heal. Vision might be good right after the procedure but gets temporarily blurrier until the epithelium grows back. Vision starts clearing up substantially by day five.
Long-term results prove how well topography-guided treatments work:
- 94% of eyes get 20/20 or better uncorrected distance visual acuity (UDVA) within six months
- 69% achieve 20/16 or better UDVA in three months
- 93% reach 20/20 or better UDVA in primary treatments
The precision of these customised treatments shows in the results – 30% of eyes see better without glasses after surgery than they did with glasses before.
Healing differences in younger vs older patients
Age plays a big role in how fast patients recover from topography-guided treatments. Younger patients (under 35) heal faster because their cells regenerate better. Clinical studies show most patients are between 26.4 and 39.5 years old.
The epithelial layer in younger patients usually heals completely in 5 days. Older patients might need up to 7 days. Everyone gets some light sensitivity, mild discomfort, and watery eyes during this time. Vision takes time to stabilise and minor symptoms fade gradually. Cell changes continue even after the epithelium closes, which affects vision quality. Younger patients’ vision stabilises faster than those over 40, who might see more changes over time.
When to expect final refraction stability
Vision stability after topography-guided treatments follows a clear pattern. Most patients need 3-6 months for full refractive stability. PRK takes longer to stabilise than LASIK. Most patients see major improvements in their vision after one month. Small changes continue as the cornea heals completely. Only 7.9% of eyes show refractive changes bigger than 0.5D between three and twelve months after treatment. This shows excellent stability over time.
Patients with mild keratoconus who get combined cross-linking might see their corneal shape improve for up to 2 years after the procedure. This happens because collagen keeps stabilising, not because the treatment is wearing off. Precision Vision London’s customised follow-up schedule tracks your progress at key recovery points. Our specialists explain what to expect at each stage. This helps ensure your recovery goes smoothly throughout your visual rehabilitation.
Managing Complex Cases and Enhancements
Complex astigmatism cases sometimes need extra refinement to achieve the best results. We combine scientific precision with patient-centred decision-making to tackle these challenging situations.
Handling residual refractive error
Small amounts of residual refractive error might remain after the original topography-guided treatments. Clinical studies that dissect topography-guided treatments reveal residual refractive astigmatism over 0.5D occurred in 11.7% of eyes with topography-modified refraction. This number jumps to 27.8% when using manifest refraction alone.
Our specialists look at each case individually and assess:
- Magnitude and stability of residual error
- Corneal thickness measurements
- Quality of vision despite residual error
- Patient’s satisfaction with current outcomes
Irregular corneas with residual error often need the custom topographical neutralisation technique. This method makes the cornea more regular instead of reducing spherical equivalent.
Enhancement planning after 3 months
Success depends heavily on the timing of enhancement procedures. We assess stability at three months post-treatment at Precision Vision London. This timeframe allows proper healing while meeting our patients’ needs for visual clarity.
Modern topography-guided treatments show remarkably low enhancement rates. Research shows only 2.2% of eyes needed enhancement within seven months. These numbers reflect both precise original treatments and careful planning. Complex astigmatism cases that need enhancement benefit from advanced software solutions like the Phorcides Analytic Engine. This tool showed better outcomes with the lowest mean error vector magnitude (0.39D) compared to manifest refraction (0.56D) or topographically measured refraction (0.47D).
Spectacle correction vs re-treatment
Minor residual error with spectacle correction sometimes works better than additional laser treatment. Several factors influence this decision:
- Corneal thickness plays a crucial role. Corneas with spherical equivalent below 6D and thinnest pachymetry above 475μm can usually receive partial refractive treatment. Those between 450-475μm with higher spherical equivalent should stay away from additional tissue removal.
- Best-corrected vision improvement potential matters too. Topography-guided PRK can reduce irregular astigmatism to boost BCVA. This holds true even if UCVA temporarily decreases and needs spectacle correction.
- Risk-benefit analysis rounds out the decision process. Post-keratoplasty patients see their astigmatism reduced to subclinical levels with topography-guided PRK. This procedure also improves higher-order aberrations, which boosts visual quality even with minor residual prescription.
We create personalised enhancement strategies by carefully weighing these factors. Our focus stays on long-term visual stability and immediate visual clarity.
Safety, Predictability, and Long-Term Outcomes
Topography-guided treatments for astigmatism demonstrate excellent safety profiles during clinical evaluation. Studies from the UK show these advanced procedures have minimal complications.
Complication rates in UK-based studies
Modern topography-guided treatments show remarkably low complication rates according to clinical data. Corneal haze, the most common side effect, usually clears up without any intervention. The 12-month follow-up revealed that 80.6% of eyes had no haze (grade 0), while only 3.2% showed grade 2 haze. Just 3.2% of cases experienced transient aseptic inflammatory infiltration that resolved naturally within four weeks. The risks have decreased further thanks to advances in transepithelial PRK.
Stability of results over 2+ years
The benefits of astigmatism correction last well into the future. Patients managed to keep their visual improvements stable during a 44-month average follow-up period that ranged from 31 to 65 months. Data collected over four years shows uncorrected distance vision improved from 0.51 to 0.65 (decimal), while corrected vision got better from 0.71 to 0.81. The keratometry readings stayed consistent, with mean values dropping from 44.95D to 43.14D for flat meridians and 49.32D to 46.28D for steep meridians across four years.
Patient satisfaction and quality of life
The quality of life improvements match the impressive clinical outcomes:
- Laser vision correction patients report 98.3% overall satisfaction
- 96.6% would opt for the procedure again
- Topography-guided LASIK patients give maximum satisfaction scores (5/5) unanimously
Patient’s night vision, glare reduction, and overall visual performance show substantial improvements.
Conclusion
Topography-guided laser treatments mark a breakthrough for patients with astigmatism and irregular corneas. This piece explores how these personalised procedures achieve better visual outcomes than conventional treatments can offer. Your cornea’s unique shape needs truly personalised care. Precision Vision London blends innovative diagnostic imaging with expert surgical planning to treat even the most complex astigmatism cases. Our results tell the story – 93% of eyes achieve 20/20 or better vision. Nearly a third of our patients see better without correction than they did with glasses or contacts.
Recovery times differ based on your treatment type and age. LASIK patients usually see quick improvements within 24-48 hours. PRK recovery moves more slowly over 5-7 days as the epithelium heals. Most patients see major improvements within a month, though full visual stability takes 3-6 months. UK studies confirm both safety and stability in long-term results. Most patients keep their visual improvements beyond four years with minimal complications. Patient satisfaction reaches 98.3%, showing how these procedures revolutionise daily activities and quality of life.
Precision Vision London leads astigmatism treatment through our complete diagnostic suite and sophisticated planning software like Phorcides. Our surgeons bring vast experience with complex corneal cases. This all-encompassing approach helps us enhance not just your vision measurements but your entire visual experience. A full consultation remains key to determine if topography-guided treatment fits your needs. Not everyone qualifies as an ideal candidate. Yet these advanced technologies now offer hope to many patients who were told laser vision correction wasn’t possible for them.
Your path to clearer vision begins by understanding your cornea’s unique characteristics. Our expert team guides you through each step – from the original assessment through personalised treatment planning and focused aftercare. Without doubt, topography-guided laser treatments have changed what’s possible for patients with astigmatism and irregular corneas. Careful candidate selection, precise diagnostic imaging, and customised treatment planning create truly life-changing visual outcomes.
Key Takeaways
Topography-guided laser treatments offer revolutionary solutions for patients with astigmatism and irregular corneas, delivering personalised care that often exceeds expectations from conventional treatments.
- Exceptional visual outcomes: 93% of patients achieve 20/20 vision or better, with 30% experiencing superior uncorrected vision compared to their previous glasses or contacts.
- Customised treatment planning: Advanced diagnostic imaging and software like Phorcides create truly personalised laser plans based on your unique corneal characteristics and visual needs.
- Multiple treatment options available: LASIK, PRK, and transepithelial PRK each offer distinct advantages depending on corneal thickness, irregularity patterns, and lifestyle requirements.
- Excellent long-term stability: Results remain stable beyond four years with 98.3% patient satisfaction rates and minimal complication rates in UK-based studies.
- Suitable for complex cases: Patients with irregular astigmatism, mild keratoconus, and post-surgical complications who were previously unsuitable for standard laser correction now have effective treatment options.
These advanced treatments represent a paradigm shift in vision correction, transforming not just your prescription but your entire visual experience through precision medicine tailored to your individual eye anatomy.
FAQs
Q1. Who is an ideal candidate for topography-guided laser eye surgery? Ideal candidates include those with irregular astigmatism, mild keratoconus, and patients experiencing complications from previous refractive surgeries. The treatment is particularly beneficial for individuals whose corneal irregularities make them unsuitable for standard laser vision correction.
Q2. How long does it take to recover from topography-guided laser treatment? Recovery time varies depending on the procedure and individual factors. LASIK patients typically experience rapid visual improvement within 24-48 hours, while PRK patients may take 5-7 days as the epithelium regenerates. Full visual stability is generally achieved within 3-6 months.
Q3. What are the success rates for topography-guided treatments? Clinical studies show impressive success rates, with 93% of eyes achieving 20/20 or better uncorrected distance visual acuity. Additionally, 30% of patients report better uncorrected vision after surgery than they had with glasses or contact lenses beforehand.
Q4. Are there any risks or side effects associated with topography-guided laser treatments? While topography-guided treatments have excellent safety profiles, some patients may experience temporary side effects such as mild corneal haze or dry eyes. Serious complications are rare, with UK-based studies reporting minimal long-term issues.
Q5. How long do the results of topography-guided laser treatment last? Long-term studies demonstrate stable results over 2+ years, with many patients maintaining improved vision beyond four years post-treatment. The stability of outcomes contributes to high patient satisfaction rates, with 98.3% of patients reporting overall satisfaction with their laser vision correction.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

