Laser eye surgery brings new hope to people battling keratoconus, a progressive eye condition. A single treatment of corneal cross-linking (CXL) can stop keratoconus from getting worse, with success rates above 90%. Your cornea stabilises after CXL, but you might need extra correction for astigmatism and myopia.
LASIK combined with corneal collagen cross-linking has emerged as an advanced treatment option for keratoconus. This powerful combination stops the disease from progressing and enhances your vision. CXL strengthens your cornea’s biomechanical stability by using riboflavin (vitamin B2) and ultraviolet-A light. The largest longitudinal study shows that CXL effectively stabilises the ectatic cornea and reduces corneal steepening in keratoconus patients.
This piece explains why combining these treatments could be right for you. You’ll learn what happens during the procedure and see how our expert surgeons at Precision Vision London use cutting-edge technology to create personalised care plans for this challenging condition.

Understanding Keratoconus and Its Impact on Vision
Keratoconus is a progressive eye condition that makes your cornea thin out and change shape over time. A good understanding of this condition helps patients manage and treat it better.
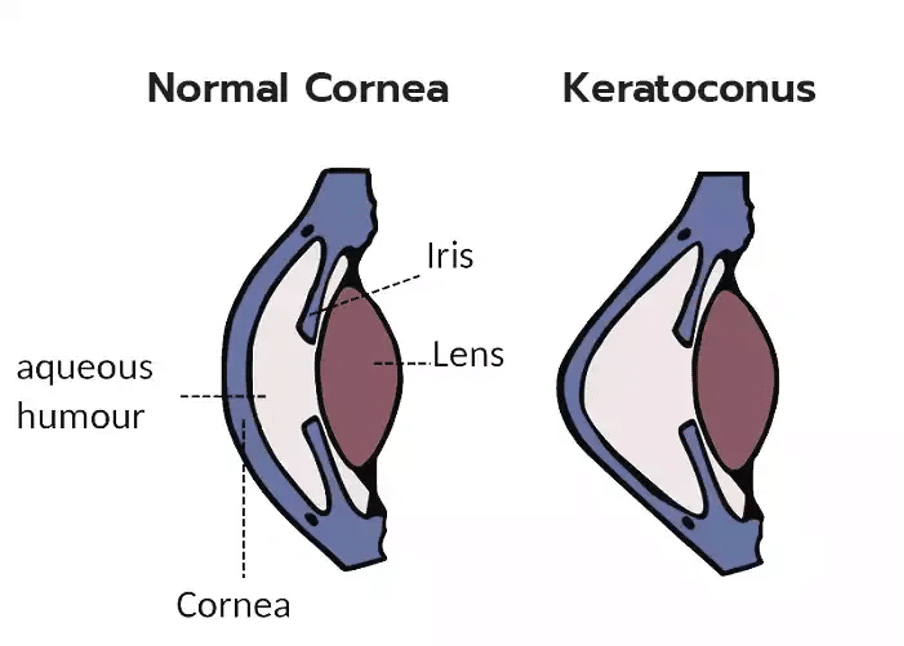
Progressive thinning and cone-shaped cornea
The central or lower central part of the cornea thins and steepens in keratoconus patients. This creates an uneven surface between the upper and lower corneal areas. Your cornea weakens and bulges outward into a cone shape instead of its normal dome shape. Both eyes usually get affected, but one eye tends to change more than the other. These corneal changes start during puberty or early adulthood. The condition can progress for 10-20 years before it stabilises around age 30-40.
Symptoms: blurred vision, glare, and contact lens intolerance
Your vision develops several problems as the cornea becomes more cone-shaped. Patients often see things as blurry or distorted. They become sensitive to bright light and struggle with glare, which makes night driving difficult. Many need frequent updates to their eyeglass prescriptions as their condition changes.
Advanced stages of keratoconus make wearing contact lenses harder. About 39% of patients can’t wear contact lenses for more than four hours at a time. The cornea’s sensitivity in the centre plays a big role in how well someone tolerates contact lenses. Less sensitive corneas make it harder to wear lenses comfortably.
Why early diagnosis is critical
Finding keratoconus early is vital for several reasons. Quick detection in its original stages lets doctors start treatments like corneal cross-linking right away. This can stop or slow down the disease. Early diagnosis helps prevent problems that come with advanced keratoconus, such as corneal scarring that makes vision worse. Detecting even mild cases becomes especially important for patients who want laser eye surgery. Using laser treatment on an undiagnosed keratoconic cornea could lead to severe progressive iatrogenic ectasia.
Quick treatment gives patients more options and helps maintain better vision, which improves their long-term outlook and quality of life. Here at Precision Vision London, we use advanced diagnostic technology to spot keratoconus in its earliest, most subtle stages.
The Role of Cross-Linking in Keratoconus Treatment
Corneal collagen cross-linking (CXL) stands out as the only proven way to stop keratoconus from getting worse. This breakthrough in eye treatment technology does more than just fix vision problems. CXL targets the root cause – unstable corneas.
How CXL halts disease progression
CXL aims to make the cornea more rigid and stops the ongoing thinning and bulging that comes with keratoconus. This innovative treatment creates new covalent bonds between nearby collagen molecules and between collagen molecules and proteoglycans in the corneal stroma. The cornea becomes stronger and better resists the forces that cause ectasia.
Clinical evidence shows remarkable results. CXL stops keratoconus from progressing in more than 90% of treated eyes. The largest longitudinal study following patients for up to 10 years backs up these impressive success rates. Patients with progressive disease now have a lower chance of needing corneal transplants, which used to be the only real solution for advanced cases.
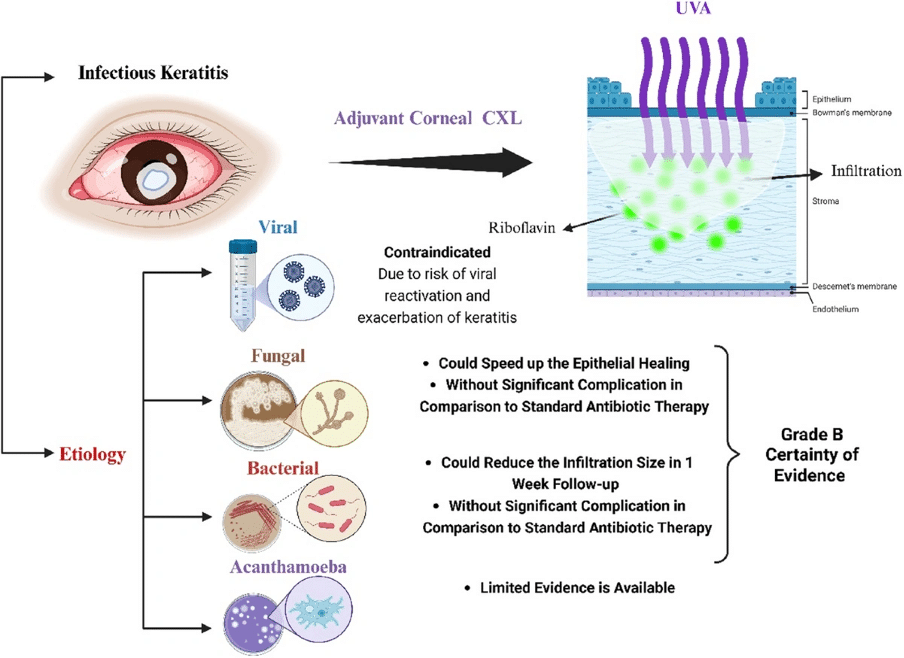
Riboflavin and UV-A mechanism explained
Two key components power the photochemical process behind CXL – riboflavin (vitamin B2) and ultraviolet-A (UVA) light. Riboflavin serves two vital functions during treatment:
- It works as a photosensitizer that creates reactive oxygen species when UVA light activates it
- It shields internal eye structures by absorbing extra UVA radiation
UVA light (370 nm wavelength) interacts with corneal tissue soaked in riboflavin. This starts both aerobic and anaerobic photochemical reactions. The aerobic phase sees activated riboflavin reacting with oxygen to create reactive oxygen species. These species help form new chemical bonds between corneal collagen fibrils. This process mirrors the natural stiffening of the cornea that happens with age, known as natural cross-linking.
Accelerated CXL protocols used at our clinic
Precision Vision London employs advanced accelerated CXL protocols. These deliver the same benefits as conventional treatment but take less time. The standard Dresden protocol used 3 mW/cm² UVA intensity for 30 minutes (5.4 J/cm² total energy). Our faster protocols follow the Bunsen-Roscoe law of photochemical reciprocity. They deliver the same energy using higher intensity over shorter periods.
Our clinic typically uses 9 mW/cm² intensity for 10 minutes or 18 mW/cm² for 5 minutes. This maintains the critical 5.4 J/cm² energy dose. These protocols work just as well as standard treatment but offer great advantages. Shorter treatment times mean better patient comfort and clinic efficiency without sacrificing results. On top of that, our pulsed light delivery system boosts oxygen availability during treatment. This makes the cross-linking effect even better.
After treatment, a clear demarcation line forms about 250-300 micrometres deep. This line marks the treatment zone. Our surgeons look for this visible sign of successful cross-linking during follow-up visits.
Why We Combine LASIK and Cross-Linking at Precision Vision London
Precision Vision London combines LASIK and cross-linking to create a substantially advanced keratoconus treatment. Keratoconus doesn’t have to limit your vision. Precision Vision London provides advanced treatment plans that combine LASIK and corneal cross-linking to boost stability and long-term clarity.
Improved visual outcomes with combined approach
The combined procedure produces better visual results than either treatment alone. Studies show patients gain approximately one line improvement in both uncorrected and best-corrected vision after combined treatment. Results indicate 70% of eyes achieve uncorrected visual acuity of 20/20 or better after LASIK-CXL. This dual approach corrects refractive errors while stabilising the disease.
Minimising risk of ectasia and regression
Traditional LASIK alone presents potential risks for keratoconic patients. Our combined technique reduces these concerns effectively. Research shows LASIK with prophylactic CXL results in less regression (+0.22D) compared to LASIK alone (+0.72D). This superior stability happens because:
- CXL strengthens the intermediate corneal stroma
- The procedure increases covalent bonding between collagen fibres
- Biomechanical stability improves substantially
Tailored treatment for mild to moderate keratoconus
This approach works best especially when you have mild to moderate keratoconus. The ideal candidates should have corneal thickness of at least 430 microns and dioptric differences of less than 10D across their cornea. These patients receive both vision correction and disease stabilisation in a single treatment session.
What to Expect Before, During and After the Procedure
Your keratoconus treatment combining LASIK and cross-linking needs a full picture to ensure the best results.
Preoperative assessment and eligibility
A complete eye examination starts your treatment journey. Advanced topography and tomography scans map your cornea’s shape, thickness, and stability. You should stop wearing rigid gas permeable contact lenses two weeks before assessment. Soft lens users need to wait one week. You’ll need a minimal corneal thickness of 400 microns and stable refraction for at least two years.
Step-by-step overview of LASIK + CXL procedure
Local anaesthetic makes this a day-case treatment. A femtosecond laser creates a thin corneal flap. The surgeon applies riboflavin solution (vitamin B2) to the exposed stromal bed after laser ablation for about 90 seconds. The flap returns to position after careful irrigation. UVA light treatment lasts 90 seconds at 30 mW/cm². A protective bandage contact lens completes the procedure.
Recovery timeline and follow-up care
Mild discomfort lasts 48-72 hours after the procedure. Your treatment includes antibiotic drops, steroids, and lubricants. The protective lens stays in place for 3-7 days until your epithelial healing finishes. Your vision should return to pre-operative levels within 7-14 days. The healing process continues for 3-6 months.
Expected visual improvements and stability
Many patients achieve 20/20 vision with improved uncorrected sight. Research shows excellent stability compared to LASIK alone – minimal regression (+0.22D vs +0.72D). The procedure stops keratoconus progression in over 90% of cases.
Conclusion
LASIK combined with corneal cross-linking has become the most important advancement for keratoconus patients. This innovative treatment targets corneal stability and vision correction at the same time. Patients who have mild to moderate keratoconus see better results with this dual approach that stops disease progression.
Clinical evidence shows how cross-linking works, stopping keratoconus advancement in over 90% of cases. The combined procedure shows less regression than other options and helps maintain stable vision over time. Your vision will improve gradually during recovery, and many patients achieve 20/20 vision after complete healing.
Precision Vision London leads pioneering keratoconus treatment with our expert surgical team and advanced diagnostic equipment. Our accelerated protocols reduce treatment time without affecting results. We take a complete approach that has detailed preoperative assessment, tailored treatment planning, and careful follow-up care to ensure the best outcomes for your eye condition.
Keratoconus patients now have new hope through advanced combined treatments. Our expert team at Precision Vision London will guide you from your original assessment through treatment and recovery. Book your consultation today to explore your tailored treatment options and achieve the clearest, most stable vision possible.
Key Takeaways
Combined LASIK and cross-linking treatment offers superior outcomes for keratoconus patients, addressing both vision correction and disease stabilisation in one comprehensive approach.
- Cross-linking halts keratoconus progression in over 90% of cases by strengthening corneal collagen fibres with riboflavin and UV-A light treatment.
- Combined LASIK-CXL delivers better visual stability with minimal regression (+0.22D) compared to LASIK alone (+0.72D), ensuring long-term results.
- Approximately 70% of patients achieve 20/20 vision or better after combined treatment, significantly improving quality of life for keratoconus sufferers.
- Early diagnosis proves critical for treatment success, as mild to moderate cases respond best to combined therapy with optimal corneal thickness requirements.
- Accelerated protocols reduce treatment time whilst maintaining effectiveness, with complete recovery typically occurring within 3-6 months post-procedure.
This innovative approach transforms keratoconus from a progressive, vision-threatening condition into a manageable eye disorder with excellent long-term prognosis and visual outcomes.
FAQs
Q1. Can corneal cross-linking improve my vision? While the primary purpose of corneal cross-linking is to halt the progression of keratoconus, many patients experience improved vision as a result. The treatment can lead to a more stable cornea, potentially reducing your eyeglass prescription and making contact lenses more comfortable to wear.
Q2. What are the main advantages of combining LASIK with cross-linking? The combined approach offers dual benefits: it corrects refractive errors while also stabilising the cornea. This results in improved visual outcomes, reduced risk of regression, and better long-term stability compared to either treatment alone.
Q3. How long does recovery take after combined LASIK and cross-linking? Most patients return to their pre-operative vision levels within 7-14 days. However, complete healing continues for 3-6 months. During this time, you’ll notice gradual improvements in your vision quality.
Q4. Am I eligible for combined LASIK and cross-linking if I have keratoconus? Eligibility depends on several factors, including the severity of your keratoconus. The treatment is most suitable for mild to moderate cases. You’ll need a minimum corneal thickness of 400 microns and a stable refraction for at least two years to be considered.
Q5. What kind of visual improvements can I expect after the combined procedure? Many patients achieve significant visual improvements, with approximately 70% reaching 20/20 vision or better. The procedure also offers excellent stability, with minimal regression compared to LASIK alone, ensuring long-lasting results.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

