Patients with high prescriptions face lens replacement problems by a lot more often. The procedure boasts an impressive success rate though. About 95% of patients don’t need glasses after surgery. But people with severe short-sightedness deal with completely different risks.
Understanding specific risks linked to high prescriptions is a vital part if you have plans for lens replacement eye surgery. The data shows permanent serious vision loss affects roughly 1 in 500 patients after refractive lens exchange. These numbers are by a lot higher than laser vision correction complications. People with high levels of myopia face bigger chances of retinal detachment – a serious issue that puts vision at risk.
Lens replacement surgery still stands as a popular choice for people over 50 who have high prescriptions. Their natural lens flexibility decreases, which makes them less ideal candidates for laser procedures. This piece will get into the complete picture of lens replacement surgery’s risks and benefits. This information helps you decide if the procedure fits your prescription strength.

What is lens replacement surgery and how does it work?
RLE stands out as one of the biggest breakthroughs in vision correction surgery, especially if you have reading glasses or high prescriptions and are over 40. This surgery has become the foundation of modern lens replacement and gives a lasting solution to many vision problems.
Understanding refractive lens exchange (RLE)
RLE, which people also call lens replacement surgery, removes your eye’s natural lens and puts in an artificial intraocular lens (IOL). Think of it as building your glasses or contact lenses right into your eyes. The surgery helps fix common vision problems like short-sightedness (myopia), long-sightedness (hyperopia), astigmatism, and presbyopia – that annoying age-related problem where you can’t focus on things up close.
RLE works differently from laser vision correction. Instead of reshaping the cornea, it changes your eye’s lens completely. This makes it a great choice if laser procedures don’t work for you because of thin corneas, dry eyes, or other corneal issues. The best part? Once you replace your natural lens with an artificial one, you can’t get cataracts later in life. People over 40 benefit most from RLE, particularly those who notice their eyes getting less flexible with age. This surgery could be your answer if glasses or contacts get in the way of your daily life.
How it differs from cataract surgery
RLE and cataract surgery use similar techniques. Both replace your eye’s natural lens with an intraocular lens implant. The main difference lies in why we do the surgery and what kind of lens we take out. Cataract surgeons remove a cloudy lens that makes everything look blurry or scattered. Their goal is to help you see clearly again. RLE takes out a healthy lens to help you depend less on glasses or contacts.
The timing also sets these surgeries apart. You get cataract surgery when poor vision starts affecting your life, but RLE is something you choose to improve your vision quality and reduce your need for glasses. Cataract patients struggle to see even with glasses on, while RLE patients see fine with their corrective lenses.
What happens during the procedure
Each eye takes about 15-30 minutes, and you can go home the same day. Before surgery, your doctor will check your eyes thoroughly and help you pick the best type of intraocular lens. Your surgeon will numb your eye with drops on surgery day. You might get something to help you relax too. You’ll stay awake but won’t feel much, and your vision will be fuzzy – just lights and movement.
Here’s what happens step by step:
- Your surgeon makes a tiny self-sealing cut where your eye’s white part meets the cornea
- They create a small circular opening to reach your natural lens
- Using ultrasound (phacoemulsification), they break up your natural lens until it’s liquid
- A vacuum system removes the broken-up lens
- Your new intraocular lens goes in through that same small cut
- The cut heals by itself without stitches
After surgery, you’ll get a protective shield for your eye. Most people head home that day and notice better vision right away, though things might look a bit blurry at first. If you need both eyes done, your surgeon will usually wait a week between surgeries. This gives your brain time to adjust to the new vision in your first eye.
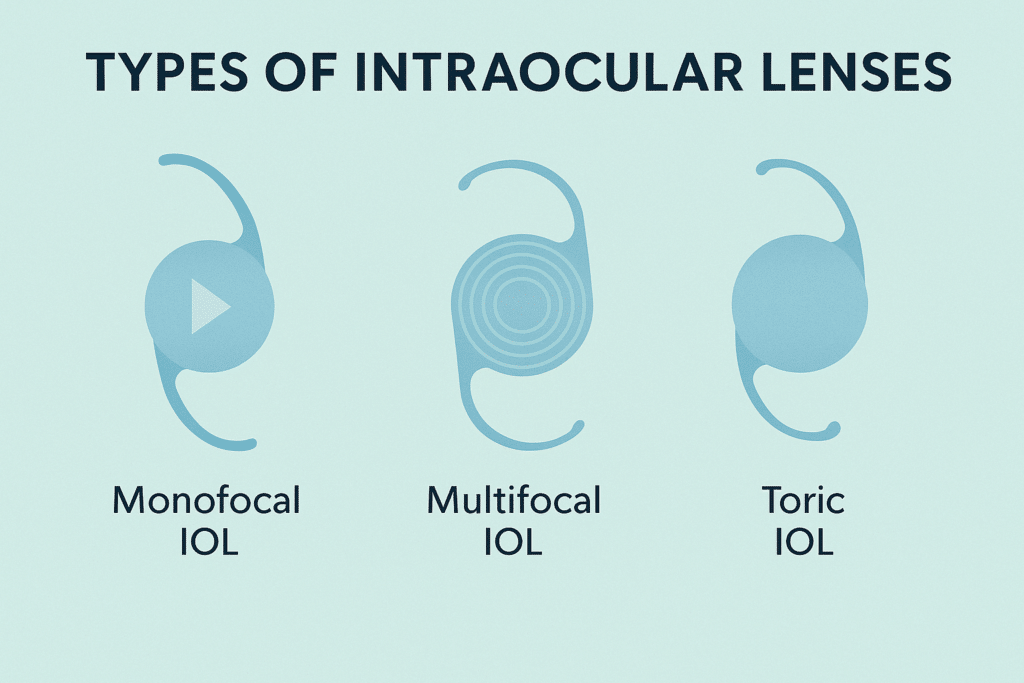
You can choose from several IOL types: monofocal lenses for either distance or near vision, multifocal and trifocal lenses for seeing at different distances, toric lenses to fix astigmatism. Your doctor will help you pick the right one based on your lifestyle and vision needs.
Why high prescriptions are treated differently
If you have extreme refractive errors, lens replacement surgery needs special attention. Your prescription’s severity affects both your eligibility for surgery and possible complications. This creates a unique risk-benefit scenario that is different from patients with mild vision problems.
What qualifies as a high prescription?
Ophthalmologists measure prescription strength in diopters (D) to determine what makes a “high” prescription. Short-sightedness (myopia) prescriptions below -5.00D are classified as severe or high myopia. Some patients’ prescriptions even measure in double digits on the negative scale.
Long-sightedness (hyperopia) becomes high when measurements go beyond +3.00D. These extreme prescriptions lead to:
- Unusually thick or heavy glasses
- Higher chances of retinal complications
- Poor night vision quality
- Total reliance on visual aids for simple daily tasks
Standard optical shops can handle most prescriptions. However, severe cases (reaching -20.00D for myopia or +20.00D for hyperopia) might need specialty lenses or other correction methods. Prescriptions over +2.00D affect activities like driving by a lot. Values beyond +5.00D associate with higher risks of various eye conditions.
Why standard lens surgery may not be enough
Traditional laser vision correction has major limits if you have extreme prescriptions. Most regular clinics can safely fix myopia only between -0.5D and -8.0D. This leaves many patients with high prescriptions without laser options. Corneal tissue requirements create the main restriction. A specialist explains: “The treatment of higher prescriptions requires more corneal tissue to be removed”. Lens replacement procedures become more challenging with high prescriptions for several reasons:
Your natural cornea’s thickness becomes crucial. It must be thick enough to handle both the surgical flap creation and tissue removal. Many patients with high prescriptions can’t get standard LASIK procedures because their corneas aren’t thick enough. Surgical results vary more with extreme prescriptions. The healing becomes less predictable and might need extra procedures to adjust results. Higher prescriptions mean less effective correction. This happens because your eye’s anatomy needs bigger changes.
Recovery takes longer if you have high prescriptions. Major changes to your eye’s structure can lead to longer adjustment times and more discomfort after surgery. Refractive lens exchange (RLE) is a chance for many patients with high prescriptions, especially those over 40. RLE works inside the eye instead of reshaping the cornea. This helps correct vision whatever your corneal thickness. As we get older, our natural lens becomes less flexible and clear. This makes lens replacement a good choice even for moderate prescriptions.
You might be right for RLE if you:
- Are 50+ (younger patients might qualify in special cases)
- Have prescriptions beyond laser surgery’s normal range
- Have presbyopia (age-related focusing problems)
- Have stable glaucoma
Patients with extreme prescriptions face more complex choices with bigger risks. The basic procedure stays similar, but risk factors, expected results, and other options need a full picture from experienced specialists who can give truly personal recommendations.
Types of lenses used in surgery
Choosing the right type of lens is one of the most important decisions in lens replacement surgery. Your choice affects your vision quality after surgery, possible side effects, and whether you’ll need glasses afterward.
Monofocal lenses
Monofocal lenses are the most popular choice for lens replacement surgery. These lenses have a single focusing power that gives clear vision at one specific distance—near, intermediate, or far. Most people choose to set their monofocal lenses for distance vision, which helps with activities like driving. The main drawback of monofocal lenses is their inability to provide clear vision at multiple distances at once. So, most people still need reading glasses for close-up work. These lenses give excellent clarity but lack versatility.
A key benefit of monofocal lenses is their reliable visual outcome with minimal disturbances. A specialist puts it this way: they deliver “sharp and crisp vision with minimal optical disturbances”. This reliability makes monofocal lenses a safe choice for patients with high prescriptions who might be prone to visual distortions.
Multifocal and trifocal lenses
Multifocal and trifocal lenses are advanced options that help reduce dependency on glasses after surgery. These advanced lenses have multiple focusing zones that let you see clearly at different distances at the same time. Trifocal lenses correct vision at three different distances: near, intermediate, and far. They work great for various tasks from reading to computer work to driving.
Multifocal lenses work by splitting incoming light, and your brain adapts to pick the right focusing power needed for each task. Research shows that 5-10% of patients might see halos or glare around lights. While this effect often decreases over time, it’s worth noting, especially for patients with high prescriptions who already face a higher risk of visual issues.
Toric lenses for astigmatism
Toric lenses fix a specific vision problem called astigmatism—a condition where the cornea or lens has an irregular curve, which causes blurry or distorted vision. Unlike regular lenses with a round surface, toric lenses look like “a slice of the side of a donut”.
Their unique design creates different focusing powers vertically and horizontally, which directly fixes the irregular curve causing astigmatism. These lenses are essential for patients whose astigmatism would stay uncorrected with standard lens replacement.
Toric lenses must stay perfectly aligned in the eye. Manufacturers add several stabilising features such as:
- Thin-thick zones
- Lens truncation (where the bottom part is slightly cut off)
- Ballasting (strategic weight distribution)
These lenses can work with any other lens type—monofocal, multifocal, or extended depth of focus—to fix astigmatism while providing other vision benefits.
Risks of lens replacement surgery for high prescriptions

Patients who need extreme prescriptions face unique challenges when they think about lens replacement surgery. The procedure lets you live without glasses, but stronger prescriptions substantially increase risks. This creates special concerns you won’t see in typical cases.
Increased risk of retinal detachment
The biggest risk for patients with high prescriptions is retinal detachment. This happens when the light-sensitive tissue at the back of your eye pulls away from its supporting layers. You need immediate medical care to prevent permanent vision loss.
If you have severe myopia (above -10D), your baseline risk of retinal problems is naturally higher. Lens replacement surgery makes this risk even worse. Research shows that retinal detachment risk jumps five times higher in the first four years after surgery. This higher risk doesn’t go away quickly—it can last and even grow for several years after the procedure.
The numbers tell a worrying story. A seven-year study of patients with myopia greater than -12D found that 8.1% had retinal detachment after clear lens extraction (up from just 2% at the four-year mark). This rate doubles the estimated detachment risk for people with severe myopia who skip surgery.
Main risk factors include:
- Young age (especially males under 60)
- Extended axial length of the eye
- Peripheral retinal degenerations
- Absence of posterior vitreous detachment
Greater chance of visual disturbances
Beyond structural complications, high-prescription patients usually see more noticeable visual disturbances after surgery. These vision quality issues can really affect how happy patients are with their results.
Common visual disturbances show up as:
- Halos and glare around lights (especially bothersome at night)
- Starbursts radiating from light sources
- Negative dysphotopsias (arc-shaped shadows in peripheral vision)
About one in 20 patients with traditional multifocal lens implants develop these visual issues. High-prescription patients might experience stronger and longer-lasting effects. These problems usually come from the type of intraocular lens used, pupil size in low light, and tiny irregularities in the optical surface.
Research also shows that switching your natural lens with an intraocular lens changes peripheral vision quality. Studies using scanning peripheral wavefront sensors showed that eyes with monofocal IOLs have larger values of oblique astigmatism in the periphery.
Higher likelihood of needing additional procedures
High-prescription patients often need follow-up procedures to fix complications or improve vision results. YAG laser capsulotomy is the most common secondary procedure. Doctors use it when the lens capsule that holds the artificial lens gets cloudy after surgery.
This condition, called posterior capsule opacification (PCO), affects about one in five patients. A seven-year study of patients with myopia greater than -12D found that over 60% needed capsulotomy for opacification. Most patients had this procedure 48 months after their original surgery.
High-prescription patients might also need:
- Laser enhancement procedures to fine-tune vision
- Lens repositioning if alignment causes visual problems
- Retinal surgery if detachment occurs
These higher risks mean patients with extreme prescriptions need detailed pre-operative counselling about possible complications. Many retina specialists worry about using multifocal IOLs in eyes with retinal diseases, including previous retinal detachment. Any future retinal complications could seriously limit vision quality and patient satisfaction.
Common side effects and how they affect recovery
The road to recovery after lens replacement surgery comes with several temporary side effects that affect your comfort and vision. Let me help you understand what to expect during your healing process.
Blurry vision and light sensitivity
Blurry vision is something almost everyone experiences after lens replacement surgery. Your vision starts out cloudy as your eye gets used to the new intraocular lens. This happens because of normal swelling after surgery. Patients with larger or denser cataracts tend to have more inflammation. Each patient’s recovery time differs. Most people see better within days, but it takes two to four weeks for vision to become stable. People who have corneal conditions like Fuchs dystrophy might deal with swelling for a month or longer.
Your eyes become more sensitive to light during recovery. This happens because:
- Your new artificial lens lets in more light than your old cloudy one
- Your pupil might not work as well right after surgery
- The healing tissue around your new lens reacts more to light
Light sensitivity usually gets better over 2-6 weeks after surgery. In spite of that, if you suddenly feel more sensitive to light and have pain, see your doctor right away as this could mean complications.
Dry eyes and discomfort
Much of lens replacement patients deal with dry eye syndrome. Research shows 42% to 64% of patients’ eyes feel dry after surgery. This happens because:
- Surgery disrupts the tear film
- The surgical cut reduces tear production
- The eye makes less mucin
Many people say their eyes feel scratchy, like there’s sand in them while healing. This usually stops within a week, but if you have dry eyes, it might last up to three months. Your surgeon will give you anti-inflammatory drops to help with dryness and swelling. If your symptoms are mild, over-the-counter preservative-free artificial tears should help.
Glare, haloes and night vision issues
Visual disturbances called dysphotopsias are common at first. The type depends on your lens and personal factors. You might see:
- Extra brightness from lights
- Rings around light sources
- Light that looks like it’s bursting
- Streaks or arcs of light
About one in 20 people who get multifocal lens implants notice these changes, especially at night. While 67% of patients see positive dysphotopsia right after surgery, only 2.2% still have it after a year.
Several things affect whether you’ll have these issues:
- The shape and design of your lens (sharp edges increase the chances)
- What your lens is made of (higher refractive index materials make it more likely)
- How big your pupil is (though studies don’t agree on this)
- The size of your lens (smaller ones raise the risk)
If you have a strong prescription and you’re thinking about lens replacement, knowing about these short-term side effects helps set the right expectations. Most issues go away as your brain adjusts to the new lenses. Talk to your surgeon if any symptoms last longer than expected – you might need additional treatment.
Rare but serious complications to be aware of
Lens replacement surgery can lead to rare but serious complications beyond regular side effects. These conditions need immediate medical attention to avoid permanent damage to your vision.
Infection and inflammation
Severe infections after surgery are rare but remain one of the biggest problems with lens replacements. Only about 0.05% of patients face the risk of severe infection. You should contact your surgeon right away if you experience any pain or sudden vision loss that needs urgent evaluation.
Your body can develop inflammation with or without an infection. Your surgeon will prescribe antibiotics or anti-inflammatory medications to reduce these risks. This becomes especially important if you have high prescriptions since existing conditions might make you more prone to inflammatory responses.
Posterior capsule rupture
A posterior capsule rupture (PCR) happens when the thin membrane holding your lens tears during the procedure. This is a big deal as it means that other risks increase significantly—a torn capsule or zonules leads to a fifteen- to seventeenfold higher risk of endophthalmitis with clear corneal incisions.
Your surgeon must quickly adjust their approach if PCR occurs:
- Stop all aspiration and ultrasound
- Maintain irrigation while preventing chamber shallowing
- Use dispersive viscoelastic to stabilise the area
- Potentially perform vitrectomy to remove any prolapsed vitreous
PCR might require a different lens placement approach since standard in-the-bag positioning could become impossible. A three-piece lens placement in the ciliary sulcus might be needed instead. Rupture cases often need extra surgery and possibly a new lens implant.
Cystoid macular oedema (CMO)
CMO stands as the most frequent cause of vision decline after lens replacement surgery. It occurs more often than retinal detachment or endophthalmitis. This condition happens when fluid builds up in your central retina (macula), which controls detailed central vision.
Doctors estimate CMO occurs in 1% to 19% of cases, though OCT imaging shows rates could reach 60-70%. Many patients notice subtle vision issues even with good results on standard Snellen charts. Common signs include:
- Blurred or distorted central vision
- Decreased visual acuity, particularly during reading
- Contrast sensitivity loss
- Colours appearing washed out
Doctors usually start treatment with topical non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroid eye drops. Oral medications or intravitreal injections might be needed for stubborn cases. “The longer CMO exists, the more permanent damage occurs in the retinal architecture”, which makes early treatment vital.
Learning about these rare but serious complications plays a vital role in evaluating lens replacement surgery risks against benefits. This becomes even more important if you have high prescriptions that might increase your chance of complications.
Alternatives to lens replacement for high prescriptions
You might worry about lens replacement surgery risks. The good news is that you have several options to correct high prescriptions. Each option works differently based on what you need for your vision.
Laser vision correction (LASIK, PRK)
Laser procedures reshape the cornea to fix vision problems. LASIK (Laser-Assisted In Situ Keratomileusis) and PRK (Photorefractive Keratectomy) are popular choices. These techniques work well for mild to moderate vision problems but have limits when it comes to extreme prescriptions. LASIK can treat prescriptions up to -8.0D, which is nowhere near enough for severe cases that reach -20D. PRK removes the outer corneal layer instead of making a flap. This makes it a better choice for patients with thinner corneas. Both methods fall short when prescriptions go beyond these ranges.
These procedures change your cornea’s normal shape. This can lead to problems like haze with PRK or flap-related issues and ectasia with LASIK. The potential risks often outweigh the benefits for very high prescriptions.
Phakic intraocular lenses (PIOLs)
PIOLs are a great option for people with extreme prescriptions. They keep your natural lens and add a synthetic one to fix your vision. These implants can treat myopia up to -23D, hyperopia to +12D, and astigmatism between 0.5 and 6.0D. The Visian ICL (intraocular collamer lens) is the most common PIOL worldwide. It sits behind your pupil but in front of your natural lens. PIOLs are perfect for patients who can’t get laser procedures because of thin corneas or high prescriptions.
Worried about your high prescription? Book a consultation with our expert surgeons to explore safe, personalised options for clearer vision at Precision Vision London.
Continuing with glasses or contact lenses
Traditional correction methods still work well as alternatives to surgery. Modern glasses fix myopia with concave lenses that move light focus back onto the retina. They’re safe but can limit active lifestyles and sports.
Contact lenses give you better peripheral vision without fogging or physical limits. Daily disposables are the safest choice for most patients. They need regular care and have a small infection risk. You should never wear them overnight as this makes infection much more likely.
Your best choice depends on your prescription, corneal features, and lifestyle needs.
How to reduce your risk and make an informed decision

Image Source: St Joseph’s Hospital
Your best defence against lens replacement problems lies in making informed decisions. Good preparation and specialist guidance will reduce risks by a lot, especially for high prescription surgeries.
Choosing the right clinic and surgeon
At Precision Vision London, our surgeons are registered with the General Medical Council and listed on the Specialist Register for ophthalmology, demonstrating their completed specialist training. Our world-renowned surgeons maintain ongoing professional development as required by professional bodies like the Royal College of Ophthalmologists.
Experience is paramount in vision correction procedures. Our lead surgeons at Precision Vision London perform hundreds of procedures each year and were among the first in the UK to perform bilateral laser surgery, remaining at the forefront of advancing vision correction. For high prescription cases that require specialist expertise due to higher complication risks, our elite surgeons bring unparalleled expertise to your ophthalmic care.
We operate from our independent, surgeon-led practice located in Harley Street, the “clinical heart” of London. Quality ratings from the Care Quality Commission (CQC) are important indicators of a clinic’s standards. The CQC evaluates safety, effectiveness, care quality, responsiveness, and leadership—all areas where Precision Vision London maintains exceptional standards through our state-of-the-art technology and premium, personalized care approach.
Pre-surgery screening and eye health checks
A complete pre-operative assessment will prepare you for surgery. This nurse-led health check helps you get ready for admission, treatment, and discharge. Your assessment will include:
- Vision testing and measurements of eye pressure, height, weight
- Blood pressure checks and urine sample analysis
- Additional investigations like heart tracings or blood tests if needed
- Special eye measurements to find the best intraocular lens
Hard contact lenses should come out two weeks before your appointment. Soft lenses need to be removed 48 hours before, as they can affect corneal readings.
Discussing lens options and expectations
Your surgeon should go through vision correction options based on your needs. You need realistic expectations during this process. One specialist puts it well: “We don’t treat a set of eyes, we must treat the whole person”. Good consultations follow five steps: understanding your wants, checking if they’re realistic, working out compromises, reaching agreement, and recording decisions.
Do you worry about your high prescription? Talk to our expert surgeons at Precision Vision London about safe, personalised options for clearer vision. The final lens choice should match your vision and lifestyle needs. You might need monofocal lenses for distance vision, multifocal options to reduce glasses use, or toric designs to correct astigmatism.
Conclusion
Lens replacement surgery can change lives for many patients. People with high prescriptions should know they face different risks. This knowledge gives you the strength to make choices that line up with your vision needs and comfort level. The biggest concern for high prescription patients is retinal detachment. The risk is about five times higher in the first four years after surgery. On top of that, these patients often notice more visual disturbances like halos and glare. They might need more time to adapt or extra procedures later.
Your lens choice becomes vital with high prescriptions. Multifocal lenses help reduce dependency on glasses but might cause more visual disturbances. Monofocal lenses offer clearer vision with fewer side effects. Many doctors call it a safer option for patients with extreme prescriptions. You should think about other options before choosing surgery. Phakic intraocular lenses keep your natural lens while fixing prescriptions up to -23D. This works well for patients who can’t get laser procedures. Modern glasses and contact lenses still provide risk-free vision correction despite their limits.
Good research matters when you think about lens replacement with a high prescription. A surgeon’s experience with extreme refractive errors can substantially lower your risk of complications. Full pre-operative screening helps spot weak areas in your retina that need treatment before surgery. Lens replacement surgery improves life quality dramatically for people with high prescriptions. The benefits are substantial but come with higher risks. Your choice should match your priorities – whether glasses-free vision is worth the risks, or if safer approaches suit you better.
FAQs
Q1. Who may not be a good candidate for lens replacement surgery? Patients with certain autoimmune diseases, those on blood-thinning medications, or individuals who have had previous eye surgeries with complications may not be suitable candidates. The surgery also carries higher risks for people with extremely high prescriptions.
Q2. What are the most serious potential complications of lens replacement surgery? While extremely rare, the most serious complications can include infection, retinal detachment, and severe inflammation. In very rare cases, these could potentially lead to permanent vision loss. However, the vast majority of patients experience successful outcomes.
Q3. Why might vision be blurry after lens replacement surgery? Blurry vision is common in the days and weeks following surgery, primarily due to normal post-operative swelling in the eye. This is usually temporary, with most patients seeing significant improvement within a few days to weeks as the eye heals.
Q4. What are some common visual disturbances after lens replacement? Some patients may experience glare, halos around lights, or difficulty with night vision, especially with multifocal lenses. These effects are often more pronounced in patients with high prescriptions but typically diminish over time as the brain adapts to the new lenses.
Q5. How does lens selection impact outcomes for high prescription patients? Lens selection is crucial for patients with high prescriptions. While multifocal lenses can reduce dependence on glasses, they may increase the risk of visual disturbances. Monofocal lenses often provide clearer vision with fewer side effects, making them a potentially safer choice for those with extreme prescriptions.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

