Patients rate refractive lens exchange surgery highly, with an impressive 95% satisfaction rate. Many patients call it a life-changing experience. This vision correction surgery provides a permanent solution that eliminates future cataract surgery needs and reduces dependence on glasses or contact lenses. You should learn about potential complications before making your decision.
Refractive lens exchange surgery comes with certain risks, though they rarely occur. Serious complications can include retinal detachment – especially when you have extreme myopia or are younger. Other risks include infection, bleeding, and increased eye pressure. The rate of permanent serious vision loss affects about 1 in 500 patients, which is substantially higher than laser vision correction.
Our team at Precision Vision London believes in giving you complete information about lens replacement surgery risks. This helps you make an informed choice about your vision correction options. This piece helps you learn about specific risks, common side effects, and ways experienced surgeons use advanced techniques to minimise these concerns.

What Makes RLE a Unique Vision Correction Option
RLE stands out among vision correction procedures. It offers a permanent solution that fixes refractive errors and stops future cataracts from developing. Let’s look at what makes it unique and understand its advantages and what it all means.
How RLE is different from cataract surgery and LASIK
RLE is similar to modern cataract surgery. Both procedures replace the natural lens with an intraocular lens (IOL). The biggest difference lies in their purpose. Cataract surgery removes a cloudy lens that impairs vision. RLE replaces a clear lens to reduce dependence on glasses or contact lenses.
LASIK works differently. It reshapes the cornea instead of replacing any eye parts. The surgeon creates a corneal flap and uses laser technology to change the corneal tissue. RLE works deeper in the eye structure. Age plays a key role in choosing the right procedure. RLE works best for patients 50 and older, especially those who struggle to focus on nearby objects due to presbyopia. Younger patients with clear, flexible natural lenses get better results from laser vision correction or phakic intraocular lens implantation.
Types of intraocular lenses used in RLE
The IOL choice affects outcomes and possible side effects:
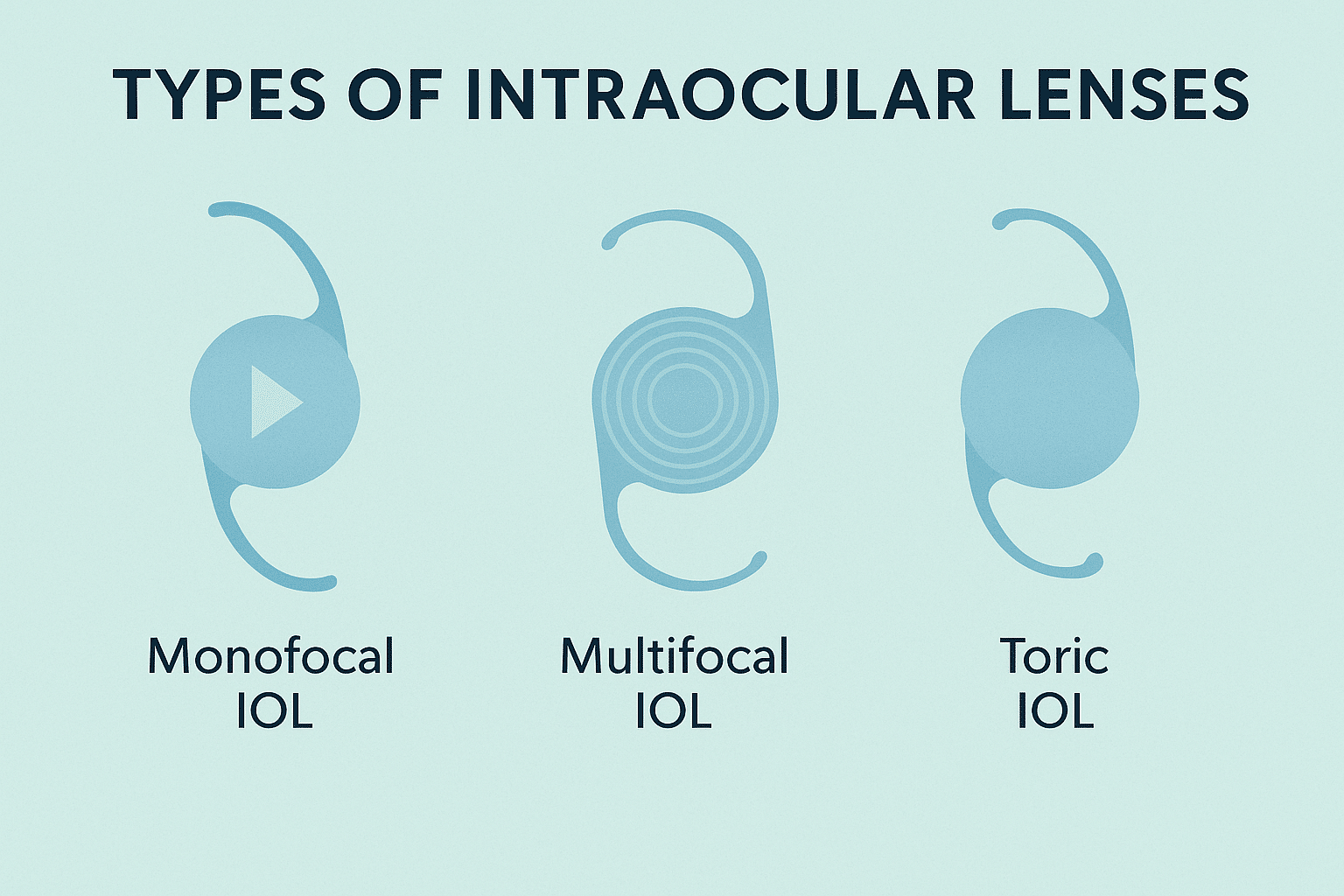
Monofocal IOLs give clear vision at one distance—usually for driving and distance vision. These basic lenses have fewer optical side effects but need reading glasses for close-up tasks.
Multifocal IOLs use different zones in the lens to provide clear vision at multiple distances. These advanced lenses substantially reduce the need for glasses for both distance and near vision.
Extended Depth of Focus (EDOF) IOLs provide better focus range than monofocal lenses. They offer good vision from distance to intermediate range with fewer visual problems than multifocal options.
Toric IOLs fix astigmatism among other refractive errors. They correct irregular corneal shapes that cause visual distortion.
Precision Vision London’s specialists help choose the right lens type. They look at your visual needs, lifestyle, and eye health to get a full picture before surgery.
Top 4 Risks of Lens Replacement Surgery Explained
Refractive lens exchange has a high success rate, but patients need to understand the potential risks to make informed decisions about their vision correction. Let’s look at four major risks that both surgeons and patients should pay attention to.
1. Retinal detachment in younger or highly myopic patients
Retinal detachment poses a serious risk for certain RLE candidates, especially when you have younger patients and those with high myopia. The risk goes up with greater axial length—each millimetre increase raises the hazard ratio for retinal detachment by 1.5. Eyes with high myopia (beyond -10.00 D) face an annual risk of retinal detachment at about 1:147. This risk jumps to roughly 1:45 after lens surgery in myopic eyes. A patient’s age plays a vital role—those 50 or younger show a higher cumulative incidence (1:27) compared to those over 50 (1:40).
2. Posterior capsule rupture and its visual effect
Posterior capsule rupture (PCR) shows up in about 4.1% of lens procedures. Patients with this complication are 3.8 times more likely to have reduced visual acuity.
Good management helps 90.6% of eyes with PCR achieve positive visual outcomes. PCR leads to higher rates of postoperative complications by a lot, including corneal oedema (0.88% vs 0.17%), endophthalmitis (0.11% vs 0.03%), and uncontrolled intraocular pressure (0.55% vs 0.03%).
3. Refractive surprise and the need for enhancement
Some patients face “refractive surprise” when outcomes differ from pre-surgical targets. Enhancement surgery after RLE happens often, affecting 16.5% of eyes in one study. Better IOL power calculations have reduced enhancement rates from 20% to 12% over six years.
4. Posterior capsule opacification and laser correction
Posterior capsule opacification (PCO), also known as “secondary cataract,” affects up to 50% of patients within five years after surgery. Younger RLE patients might see higher rates than traditional cataract patients. Vision clarity returns with a quick, outpatient YAG laser procedure to treat PCO. The YAG treatment is generally safe, but rare complications include retinal detachment (especially in highly myopic eyes), increased eye pressure, and inflammation.
Understanding Visual Side Effects After RLE
RLE patients usually notice temporary visual changes as their eyes adapt to their new intraocular lenses. Their visual acuity improves, but some optical side effects need time and understanding.
Halos and glare in low-light conditions
Light scatter effects appear in almost all patients during the early months after surgery. Bright light sources create halos—rings of light around them—and glare makes it hard to see clearly, especially when driving or at night. Most patients see these effects fade within weeks, though some might need 3-6 months to adjust fully.
Premium lenses create an interesting balance: multifocal IOLs reduce dependency on glasses but create more optical side effects than monofocal lenses. Clinical data shows 19 out of 20 patients report satisfaction with their vision 3-6 months after multifocal IOL implantation.

Peripheral shadows and shimmering arcs
RLE patients often notice distinctive shadows or shimmering light arcs in their peripheral vision. These effects, called dysphotopsias, appear in two ways:
- Negative dysphotopsias create unwanted shadows in the temporal visual field. About 12% of patients experience this one month after surgery, dropping to 3% after a year.
- Positive dysphotopsias show up as bright streaks, flashes, or light arcs in peripheral vision. Up to 67% of patients notice these effects right after surgery.
Your IOL’s design and size play a crucial role in these visual artefacts. Studies indicate that larger 7.0mm optic diameter IOLs might reduce symptoms better than standard 6.0mm optics.
Why some patients may need IOL exchange
Success rates are high, yet about 1% of patients can’t adjust to visual side effects and need IOL exchange. This usually means switching from a multifocal to a monofocal lens.
Precision Vision London’s team monitors each patient’s adaptation carefully. Our specialists can explore IOL exchange options if visual effects persist and affect quality of life substantially. Patients with an intact posterior capsule and good zonular support see the best results from this procedure. Note that visual side effects become less noticeable over time. Your brain’s neuroadaptation process keeps improving visual comfort as time passes.
How Precision Vision London Minimises RLE Risks
Safety is our highest priority for every refractive lens exchange procedure at Precision Vision London. We use innovative technology and proven protocols to reduce refractive lens exchange risks and achieve the best visual outcomes.
Advanced biometry and IOL selection for accurate outcomes
Our state-of-the-art optical biometry ensures precise lens power calculations. Modern swept-source biometers are five times more accurate (0.01–0.02 mm) than ultrasound methods. This significantly reduces the risk of refractive surprise. Our specialists use advanced formulas like Holladay 2 that factor in corneal diameter and lens thickness measurements for better predictability.
We make specialised adjustments for eyes with unusual measurements. The Wang-Koch adjustment helps prevent post-operative visual disappointment in patients with longer axial lengths.
Experienced surgeons with low complication rates
A surgeon’s expertise plays a crucial role in safety outcomes. Our specialists’ posterior capsule rupture rate is well below the national average of 4.1%. Their exceptional surgical precision leads to fewer post-operative complications, including lower risks of corneal oedema, endophthalmitis, and uncontrolled intraocular pressure.
Personalised pre-op assessments and post-op care plans
Each RLE trip starts with a detailed evaluation. We look beyond standard measurements to assess:
- Detailed corneal topography to map astigmatism
- Wavefront analysis for higher-order aberrations
- Pupillometry in varied lighting conditions
- Full retinal examinations with OCT imaging
These careful assessments help us spot potential complications early. Our well-laid-out aftercare programme provides regular follow-up appointments and 24-hour support.
Use of modern surgical techniques and safety protocols
Our operating room safety protocols go beyond industry standards. Patients choosing same-day bilateral surgery benefit from strict measures such as:
- Complete re-scrubbing and re-gowning between eyes
- Fresh instruments for the second eye
- Different batch numbers for all surgical materials
Every procedure carries risks—but at Precision Vision London, you’ll be fully informed and in expert hands. Find out if refractive lens exchange is right for you—book your personal consultation today.
Conclusion
Patients must weigh the risks and benefits of refractive lens exchange before choosing this vision-correcting procedure. Complications like retinal detachment and posterior capsule rupture rarely happen. Understanding these possibilities will help you make informed decisions about your eye health. Most patients notice temporary visual effects such as halos or peripheral shadows. These effects usually fade within 3-6 months as neuroadaptation takes place.
Precision Vision London pioneers refractive lens surgery with complete safeguards that reduce complications by a lot. Advanced biometry technology and IOL selection techniques will give remarkable accuracy in surgical outcomes. The expert surgeons maintain lower complication rates than national averages. They also follow strict safety protocols that go beyond industry standards.
Your experience at Precision Vision London starts with detailed pre-operative assessments. These include corneal topography, wavefront analysis, and full retinal examinations. This approach helps identify and resolve potential concerns before they affect your outcome. Well-laid-out aftercare programmes give you peace of mind during recovery.
Every surgical procedure has some risks. The life-changing benefits of refractive lens exchange make it worth considering. Freedom from glasses and prevention of future cataract surgery explain why patient satisfaction rates stay exceptional. Find out if refractive lens exchange suits your needs—book your personalised consultation today.
Key Takeaways
Understanding the risks and benefits of refractive lens exchange helps you make an informed decision about this permanent vision correction solution that boasts a 95% patient satisfaction rate.
- Serious complications are rare but real: Retinal detachment affects 1 in 45 highly myopic patients, whilst permanent vision loss occurs in 1 in 500 cases overall.
- Visual side effects typically resolve within 3-6 months: Halos, glare, and peripheral shadows are common initially but fade as your brain adapts to the new lens.
- Advanced technology dramatically reduces risks: Modern biometry offers five times greater accuracy than older methods, significantly minimising refractive surprises.
- Surgeon expertise matters significantly: Experienced surgeons maintain complication rates well below the 4.1% national average for posterior capsule rupture.
- Comprehensive pre-operative assessment is crucial: Detailed corneal mapping, wavefront analysis, and retinal examinations help identify potential complications before surgery.
The key to successful RLE lies in choosing an experienced surgical team that combines cutting-edge technology with rigorous safety protocols, ensuring you receive the highest standard of care throughout your vision correction journey.
FAQs
Q1. What is the success rate of refractive lens exchange surgery? Refractive lens exchange has a high success rate, with approximately 95% of patients reporting satisfaction with the procedure. However, like any surgery, it does carry some risks that patients should be aware of before deciding to undergo the treatment.
Q2. How long does it take to recover from refractive lens exchange? Most patients experience improved vision within a few days after surgery. However, complete visual adaptation, including the resolution of side effects like halos and glare, typically takes 3-6 months as the brain adjusts to the new intraocular lenses.
Q3. What are the most common side effects of refractive lens exchange? The most common side effects include temporary visual phenomena such as halos around lights, glare in bright conditions, and peripheral shadows or shimmering arcs. These effects usually diminish over time as the eyes and brain adapt to the new lenses.
Q4. Is refractive lens exchange suitable for everyone? Refractive lens exchange is generally most beneficial for patients aged 50 or over, especially those experiencing presbyopia. Younger patients with clear, flexible natural lenses may be better suited to other vision correction options. A thorough pre-operative assessment is crucial to determine suitability.
Q5. How does refractive lens exchange compare to LASIK? While both procedures aim to correct vision, they work differently. RLE replaces the eye’s natural lens with an artificial intraocular lens, addressing refractive errors and preventing future cataracts. LASIK, on the other hand, reshapes the cornea. RLE is typically more suitable for older patients or those with certain eye conditions that make them unsuitable for LASIK.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.

