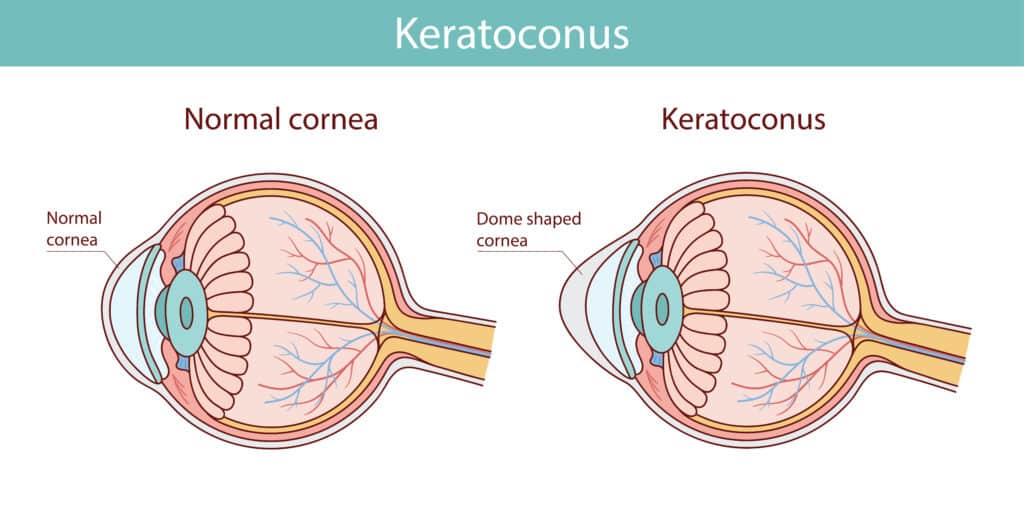
What is Keratoconus? The cornea thins and bulges outward in this degenerative disease. Instead of keeping its standard dome structure, it takes on a cone-like shape. Keratoconus creates a real challenge for anyone considering laser eye surgery. Keratoconus affects between 50 and 200 out of every 100,000 people. Many people don’t know about this eye condition until it affects their vision. Medical guidelines around the world list keratoconus as a deal-breaker for standard laser procedures. The reason is simple – LASIK creates a thin flap in the cornea and removes tissue from the inner layers.
This process could make an already weak cornea even more unstable. Eye doctors often discover Keratoconus during laser surgery screenings because its early symptoms can be subtle. The good news? Even though traditional laser eye surgery might not work, other treatment options can help. Take corneal cross-linking (CXL) for example – it makes the cornea stronger and stops further thinning or bulging. This gives your eyes better structural stability. Once you understand Keratoconus better, you can find vision correction solutions that match your needs.

What is Keratoconus, and how does it affect vision
The term keratoconus comes from Greek words that mean “cone-shaped cornea.” This eye condition affects the cornea, the clear, dome-shaped window at the front of your eye. The cornea gets thinner and weaker over time, which makes it bulge outward into an irregular cone shape instead of staying in its normal, rounded dome structure. Your cornea plays a vital role in focusing light onto the retina to give you clear vision. The bulging from Keratoconus distorts light as it enters your eye. This prevents proper focusing and leads to vision problems.
Most people develop Keratoconus during puberty, and it keeps getting worse through their 20s and 30s. Some cases show progression even after age 30. The condition usually affects both eyes but not equally, one eye often has more severe symptoms than the other. Some rare cases affect just one eye. The number of people with Keratoconus varies a lot by region. It ranges from as low as 0.0003% in Russia to as high as 5.3% in male Arab students in Israel. A large Dutch study found it affects 1 in 375 people (0.27%). A newer study from Australia showed a higher rate of 1.2% using specialised imaging.
Symptoms: What is the keratoconus symptoms profile?
You’ll notice keratoconus symptoms develop slowly, and they can be different for each person. As your condition gets worse, you might experience:
- Vision that gets worse gradually in one or both eyes
- Blurry and distorted vision where straight lines look curved
- More sensitivity to bright lights and glare
- Double vision in just one eye
- Lights surrounded by halos
- Problems seeing at night or in dim light
- Your eyeglass prescription changes often
- Your eyes feel strained, you get headaches, or you feel tired
These symptoms usually get worse over 10-20 years. At first, you might just notice slightly blurry vision or vision problems that glasses don’t fix well. The changes in your cornea become more evident as the condition advances. Keratoconus creates irregular astigmatism, which makes it hard to correct with regular eyeglasses. Later on, some people develop scarring on their cornea. This reduces how clear the cornea is and makes vision even worse.
Causes and risk factors of Keratoconus
Scientists haven’t pinpointed the exact cause of Keratoconus yet. Still, they think it comes from a mix of genetic, environmental, biomechanical, and biochemical factors.
- Genetic factors matter a lot—about 6-8% of cases run in families. Your risk goes up if you have a close relative with the condition. Research shows that having a family history of Keratoconus makes you about 25 times more likely to develop it.
- Eye rubbing has a strong link to getting and worsening Keratoconus. Studies show that rubbing your eyes often makes you 4 times more likely to develop the condition. People with allergies that make their eyes itchy face a higher risk.
These conditions also raise your risk of Keratoconus:
- Atopic conditions like asthma, eczema, and allergic rhinitis
- Down syndrome
- Connective tissue disorders like Ehlers-Danlos syndrome
- Leber’s congenital amaurosis
- Osteogenesis imperfecta
Research shows that having related parents increased the risk by about 3 times in one study. Wearing rigid gas-permeable contact lenses might also contribute to the developing of Keratoconus. Knowing these risk factors helps doctors identify who needs earlier screening and monitoring, especially before they consider laser eye surgery.
Why Standard Laser Eye Surgery is Not an Option
LASIK eye surgery can be dangerous if you have Keratoconus. You need to understand both the procedure and how it affects this corneal condition.
How LASIK works and why it’s risky for Keratoconus
LASIK (Laser-Assisted In Situ Keratomileusis) creates a thin flap in the cornea. A laser removes tissue from the inner layers to reshape the cornea. This helps correct refractive errors like nearsightedness, farsightedness, and astigmatism. The process makes the cornea thinner by design. The procedure poses serious dangers if you have Keratoconus. Your cornea is already weak and getting thinner due to the condition. LASIK removes even more corneal tissue, which makes an already unstable structure weaker. Eye surgeons consider this combination so dangerous that it’s an absolute contraindication. Medical experts agree that Keratoconus, even mild cases, is an absolute contraindication to LASIK or PRK procedures. Doctors should never perform this surgery, whatever the patient’s wishes or other factors might be.
Structural instability and risk of worsening vision
Post-LASIK ectasia is the biggest problem with performing LASIK on keratoconus patients. This condition looks like a faster form of Keratoconus that the surgery triggers. The reported incidence of ectasia after LASIK ranges from 0.04% to 0.6% in the general population, but this risk skyrockets for people with undiagnosed Keratoconus.
LASIK on a keratoconus-weakened cornea can cause:
- Faster outward bulging of the cornea after surgery
- Vision that gets worse instead of better
- Progressive steepening or thinning of the cornea
- The need for speciality contact lenses to see clearly
- Corneal transplants in severe cases
The LASIK flap provides nowhere near enough tensile strength to the cornea. Dr John Marshall, a renowned ophthalmologist, points out that LASIK can weaken the cornea by 15% to 25% in normal patients. This extra weakening becomes catastrophic for keratoconus patients.
Screening protocols at Precision Vision London
A complete picture of keratoconus screening is the lifeblood of our pre-operative assessment at Precision Vision London. Our specialists know how vital it is to spot even subtle signs of Keratoconus before refractive surgery to keep patients safe.
Our detailed screening approach uses multiple advanced diagnostic tools, since no single test can rule out Keratoconus safely:
- Corneal topography: Creates detailed, colour-coded maps showing the cornea’s surface shape and curvature, revealing patterns that indicate early Keratoconus
- Corneal tomography: Maps both front and back corneal surfaces in three dimensions—crucial since the back surface often shows changes earlier than the front in Keratoconus
- Pachymetry: Precisely measures corneal thickness at multiple points, identifying thinning patterns characteristic of Keratoconus
Soft contact lens wearers need to stop wearing them several days before testing. Rigid lens wearers usually need several weeks without lenses to get accurate results. These careful screening protocols help our specialists spot subtle corneal irregularities that might go unnoticed. This ensures we never recommend laser eye surgery to patients who could be harmed by it.
Safe and Effective Treatments for Keratoconus
Standard laser eye surgery doesn’t work for keratoconus patients. However, patients can choose from several treatments that manage this progressive condition. These treatments aim to stop progression or enhance vision without damaging the cornea.

Corneal cross-linking (CXL) to stop progression
CXL is a breakthrough treatment that makes the cornea stronger and prevents Keratoconus from getting worse. This simple procedure uses ultraviolet light with riboflavin (vitamin B2) eye drops. Together, they create new collagen bonds in the cornea to increase its strength. The treatment replicates the natural age-related cross-linking that happens after age 30. Clinical trials show CXL stops keratoconus progression in more than 90% of treated eyes. Results over the last 10 years show the same high success rates in preventing further damage. Our team at Precision Vision London uses the accelerated ‘epithelium-off’ CXL method. This updated approach delivers the same UV light energy in eight minutes instead of 30. The results are just as good, and it might even be safer.
Specialist contact lenses: RGP, scleral, hybrid
Specially designed contact lenses help many keratoconus patients see better. These lenses are different from regular ones because they work with the irregular corneal shape:
- Rigid Gas Permeable (RGP) lenses are the top choice for most keratoconus patients. These lenses create a smooth surface over the irregular cornea and neutralise visual distortion. A tear layer forms between the lens and cornea, which helps patients see clearly.
- Scleral lenses work exceptionally well for moderate to advanced cases. These bigger lenses completely cover the cornea and sit on the eye’s white part (sclera). This design keeps the sensitive cornea safe and stays in place better. Research shows these lenses helped 80% of severe keratoconus patients avoid corneal transplants.
- Hybrid lenses mix the best features of rigid and soft lenses. They have a rigid centre with a soft, comfortable outer ring that helps patients see clearly and feel comfortable. These lenses work great for patients who find RGP lenses uncomfortable or who have trouble keeping them in place.

Corneal ring segments and partial transplants
Intracorneal ring segments (ICRS) reshape the keratoconic cornea. Doctors place these small, arc-shaped implants into the corneal stroma to flatten and smooth out the central cornea. Surgeons have used ICRS in more than 500,000 eyes worldwide with an excellent safety record. ICRS works by changing the local curvature to flatten the cone-shaped bulge. This mechanical change doesn’t fix the underlying biochemical problems, but makes the corneal shape and vision much better. About two-thirds of patients see better after getting ICRS implants. Partial thickness corneal transplants (DALK) get great results when other treatments don’t work well enough. This targeted replacement keeps the deepest corneal layers and fixes the abnormal shape. Most patients’ vision improves dramatically, and about 80% can drive within a year after surgery.
Advanced Laser Options After CXL Stabilisation
Keratoconus patients can access advanced laser options after successful corneal cross-linking (CXL). These new refinements were not possible before.
Topography-guided PRK for visual refinement
Topography-guided PRK is a game-changer for patients with stable Keratoconus. The procedure creates a custom laser pattern based on detailed corneal maps. This smooths out irregularities while keeping as much corneal tissue as possible. The treatment targets specific corneal problems that cause vision distortion and lead to better overall vision. Research shows patients can improve best-corrected visual acuity by approximately two lines on vision charts.
PTK + PRK for irregular corneal surfaces
Patients with more severe corneal irregularities benefit from combining phototherapeutic keratectomy (PTK) with PRK. This two-step approach removes irregular epithelium through PTK before reshaping the underlying tissue with PRK. The treatment can reduce corneal irregularities by up to 5.0 D. Many patients can switch from rigid gas-permeable lenses to more comfortable soft contact lenses.
Expected outcomes: clarity, reduced glare, better lens fit
These procedures show remarkable visual improvements in clinical outcomes. Patients experience less ghosting, fewer halos, and reduced glare. Night vision also gets better. Studies show 70% of treated eyes achieve 20/20 or better vision without correction. The smoother corneal surface helps patients tolerate contact lenses better when they need additional correction. These sophisticated treatment options give keratoconus patients better visual results beyond just stabilising their condition.
Personalised Care at Precision Vision London
Personalised care is the lifeblood of our keratoconus management philosophy at Precision Vision London. Your trip with us starts with a complete evaluation that we customise to your specific eye condition.

How we assess suitability for laser eye surgery for Keratoconus
A complete picture of Keratoconus requires detailed examination. Our screening process has a detailed medical history review and specialised testing. Contact lens wearers must discontinue use, two weeks for rigid gas permeable lenses, one week for soft contacts. This step will give a clear and accurate reading during your assessment.
Our technology for corneal mapping and diagnostics
We use advanced diagnostics to map highly distorted corneas with perfect precision. Our complete suite has:
- Corneal topography: Creates detailed maps showing surface irregularities
- Corneal tomography: Captures three-dimensional imagery of both front and back corneal surfaces
- AI-powered technology: Boosts diagnostic accuracy for keratoconus detection
These tools help us learn about corneal changes and make informed treatment decisions.
Tailored treatment plans and long-term monitoring
We can develop custom laser treatment plans to normalise corneal irregularities after stabilising your Keratoconus with cross-linking. Regular monitoring plays a vital role, we recommend follow-up appointments every 3-6 months to assess corneal shape and thickness. This proactive approach lets us intervene quickly when needed. Our specialists stay committed to your physical eye health and emotional well-being throughout your care. We understand that facing Keratoconus can feel overwhelming, but with proper support, you can manage it effectively.
Conclusion
Keratoconus creates unique challenges when you think about vision correction options. You have learned about this progressive condition that affects your cornea’s structure and stability in this piece. Conventional laser eye surgery isn’t suitable for keratoconus patients. Still, many effective alternatives can stabilise your condition and improve your vision by a lot. A better understanding of Keratoconus leads to smarter management decisions. Of course, early detection through complete screening helps prevent vision deterioration. Precision Vision London’s advanced diagnostic technology will give accurate identification of even subtle corneal changes. This allows timely intervention before the condition worsens.
Corneal cross-linking has, without doubt, transformed keratoconus treatment by stopping progression in over 90% of cases. This breakthrough procedure, paired with specialised contact lens options, gives excellent visual outcomes for most patients. The possibility of advanced laser treatments after successful stabilisation brings hope for visual refinement that seemed impossible before. Your trip with Keratoconus needs expert guidance and personalised care. Precision Vision London’s all-encompassing approach will give you tailored treatment plans based on your specific needs. Success depends on regular monitoring, and follow-up appointments help adjust your care plan when needed.
Modern advancements have created new possibilities for keratoconus patients. Early intervention, stabilisation through cross-linking, and potential refinement with topography-guided treatments create a clear path to better vision and quality of life. Expert management at Precision Vision London helps you look forward to clearer vision and a brighter future, despite this challenging condition.
Key Takeaways
Understanding Keratoconus and its impact on laser eye surgery options is crucial for making informed vision correction decisions.
- Keratoconus causes corneal thinning and bulging, making standard LASIK absolutely contraindicated due to the risk of severe complications
- Corneal cross-linking (CXL) successfully halts keratoconus progression in over 90% of cases, strengthening the cornea’s structure
- Specialist contact lenses (RGP, scleral, hybrid) provide excellent vision correction for Keratoconus without surgical risks
- Advanced laser treatments become possible after CXL stabilisation, with 70% achieving 20/20 vision or better
- Comprehensive screening using corneal topography and tomography is essential before any refractive surgery consideration
Whilst conventional laser eye surgery isn’t suitable for keratoconus patients, modern treatments offer excellent outcomes. The key lies in proper diagnosis, stabilisation through cross-linking, and personalised treatment plans that may include advanced laser options once the condition is controlled.
FAQs
Q1. Is laser eye surgery possible for individuals with Keratoconus? Standard laser eye surgery is not recommended for people with Keratoconus due to the risk of further weakening the cornea. However, after stabilisation with corneal cross-linking, some advanced laser treatments may become possible to refine vision under careful medical supervision.
Q2. What are the main symptoms of Keratoconus? The primary symptoms of Keratoconus include gradually worsening vision, blurred and distorted sight, increased sensitivity to light, seeing halos around lights, and difficulty with night vision. Frequent changes in eyeglass prescriptions may also indicate the condition.
Q3. How effective is corneal cross-linking (CXL) in treating Keratoconus? Corneal cross-linking is highly effective in halting the progression of Keratoconus. Clinical trials have shown that CXL successfully stops the condition from worsening in over 90% of treated eyes, with long-term results demonstrating sustained effectiveness for up to 10 years.
Q4. What types of contact lenses are best for keratoconus patients? Specialised contact lenses designed for Keratoconus include rigid gas permeable (RGP) lenses, scleral lenses, and hybrid lenses. RGP lenses are often the first choice, while scleral lenses can be particularly beneficial for moderate to advanced cases, helping many patients avoid corneal transplantation.
Q5. How often should keratoconus patients have follow-up appointments? Regular monitoring is crucial for managing Keratoconus. It’s generally recommended that patients have follow-up appointments every 3-6 months to evaluate corneal shape and thickness. This allows for timely intervention if any changes occur in the condition.
Authors & Reviewer
-
 Olivia: Author
Olivia: AuthorHi, I'm Olivia, a passionate writer specialising in eye care, vision health, and the latest advancements in optometry. I strive to craft informative and engaging articles that help readers make informed decisions about their eye health. With a keen eye for detail and a commitment to delivering accurate, research-backed content, I aim to educate and inspire through every piece I write.
-
 Dr. CT Pillai: Reviewer
Dr. CT Pillai: ReviewerDr. CT Pillai is a globally recognised ophthalmologist with over 30 years of experience, specialising in refractive surgery and general ophthalmology. Renowned for performing over 50,000 successful laser procedures.
